Distress, Pain, and Coping Strategies in Patients Undergoing Breast-Conserving Surgery: A Scoping Literature Review
Problem Identification: Most patients with breast cancer are diagnosed at an early stage, when surgery remains the primary treatment. This scoping literature review explores the frequency and severity of symptoms; which patients are at the highest risk for pain, nausea, and distress; and the relationships between coping strategies and these symptoms.
Literature Review: This review included articles found in the MEDLINE®, CINAHL®, PubMed®, PsycINFO®, APA PsycArticles®, and Cochrane Library databases and published from 2010 through 2022, using combinations of the following keywords: coping, cancer, distress, surgery, and breast.
Data Evaluation: Initial search results yielded 111 research articles, and 13 were included in the review. Extracted data included the purpose, study design, sample size, time point, instrument, and conclusion.
Synthesis: Nausea, pain, and distress are substantial problems for women following breast cancer surgery. The relationships among predictors, pain, nausea, and distress are clear, but the direction and strength of these relationships remain unknown. A better understanding of the relationships among these factors is important to improve the experience of women with breast cancer.
Implications for Research: Nursing research should focus on developing targeted interventions to reduce these symptoms.
Jump to a section
In the United States, breast cancer is the most common cancer diagnosis among women. One in eight women will experience breast cancer in her lifetime (Siegel et al., 2023). Most women with breast cancer are diagnosed at an early stage (stage I or II), when surgery remains the primary treatment (Giaquinto et al., 2022). More than half of patients with early-stage breast cancer undergo breast-conserving therapy, which consists of breast-conserving surgery (also known as a lumpectomy) followed by adjuvant radiation therapy (DeSantis et al., 2019). In addition to the surgical removal of the breast tumor, these surgeries include pathology procedures that provide diagnostic information to guide the next treatment steps. However, these pathology results can take as long as two weeks before they are completed and reported back to the patient. Consequently, during this initial treatment period, women with breast cancer must recover from surgery while also awaiting results that will determine the next steps in a complicated treatment algorithm, adding to their already high levels of stress related to a recent breast cancer diagnosis.
Although it is surgically less invasive, patients undergoing breast-conserving surgery still encounter physical and psychological symptoms and require coping strategies to deal with their diagnosis and surgery. In addition, the retention of any breast tissue can, for some women, perpetuate the fear of cancer recurrence, leading to longer-term psychological symptoms (Agarwal et al., 2014; Chatterjee et al., 2015; Hartmann-Johnsen et al., 2015; Hwang et al., 2013). The surgical removal of cancer and the additional diagnostic procedures require anesthesia. The combination of anesthesia and physical tissue damage frequently causes symptoms of pain, nausea, and additional sources of distress. The National Comprehensive Cancer Network (NCCN) Guidelines for Distress Management state that psychological distress should be recognized, monitored, documented, and treated promptly at all stages of disease and in all settings (NCCN, 2023). Distress extends along a continuum and is described as the multifactorial unpleasant experience of a psychological, social, spiritual, or physical nature that may interfere with one’s ability to cope effectively with cancer, its physical symptoms, and its treatment (NCCN, 2023). As more surgeries move to the outpatient setting, the assessment and treatment of distress and associated symptoms following surgery moves from the hospital setting to the home, introducing new complexities.
Background
The vast majority of research literature addressing psychological distress, pain, and postoperative nausea and vomiting (PONV) following breast cancer surgery focuses on patients undergoing total mastectomy procedures or plastic reconstruction (Majumdar et al., 2021, 2022). In addition, most of the literature does not focus on the acute symptoms that occur on postoperative day 1. Therefore, an examination of the literature to better understand the physical and psychological experience of women undergoing breast-conserving surgery is required. A scoping review was selected to identify the gaps in the literature and provide guidance for future research (Arksey & O’Malley, 2005).
The purpose of this scoping literature review was to determine the frequency and severity of symptoms; identify the patients at the highest risk for pain, nausea, and distress; explore the relationships between coping strategies and these symptoms to capture emerging knowledge; identify where scientific advancement is required; and assist with development of future interventions to address these symptoms.
Methods
Using the methods described by Arksey and O’Malley (2005), this scoping literature review explored the relationships between distress, pain, and coping strategies in patients undergoing breast-conserving surgery. The process included identifying the research question, assessing relevant studies, selecting the studies, charting the data, summarizing the data, and reporting results. The following research questions were identified for this process:
- What are the frequency and severity of symptoms?
- What are the predictors for severe pain, nausea, and distress in this population?
- What are the relationships between coping strategies and these symptoms in women undergoing breast-conserving surgery to treat cancer?
Literature Search Strategy
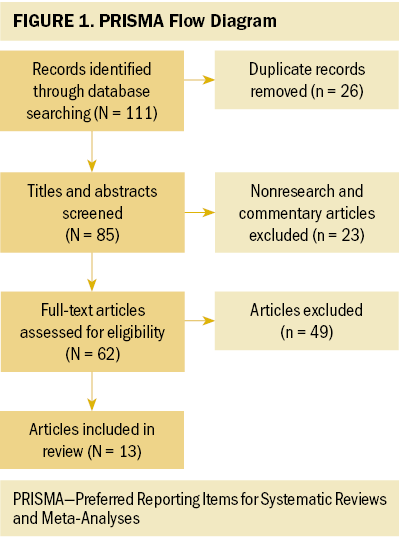
The search included the MEDLINE®, CINAHL®, PubMed®, and Cochrane Library databases. The search also included PsycINFO® and APA PsycArticles® to help reveal information regarding distress and coping strategies. The following search terms were used based on MeSH (Medical Subject Headings) descriptors: coping, cancer, distress, surgery, and breast. The search was not limited to breast-conserving surgery. The date restrictions included only literature published between 2010 and 2022. The search included systematic reviews and meta-analyses, peer-reviewed journal articles, textbooks, government reports for incidence statistics, position statements, and dissertations. The search also included Boolean operators such as “or” and “and.” The review also included ancillary or related research when necessary. The initial search results yielded 111 research articles for review (see Figure 1). After removing 26 duplicates, 85 articles were included in the initial screening. An additional 23 articles were identified as nonresearch or commentary articles and removed. Sixty-two full-text articles were reviewed. Ultimately, 13 quantitative studies met the criteria of having participants aged 18 years or older undergoing breast cancer surgery and of examining distress, pain, or coping strategies.
Findings
Frequency and Severity of Symptoms
The first part of this section discusses the frequency of pain, distress, and nausea as well as coping strategies in women undergoing breast cancer surgery. The discussion is arranged chronologically to present foundational research before the most recent literature on each subject (see Table 1).
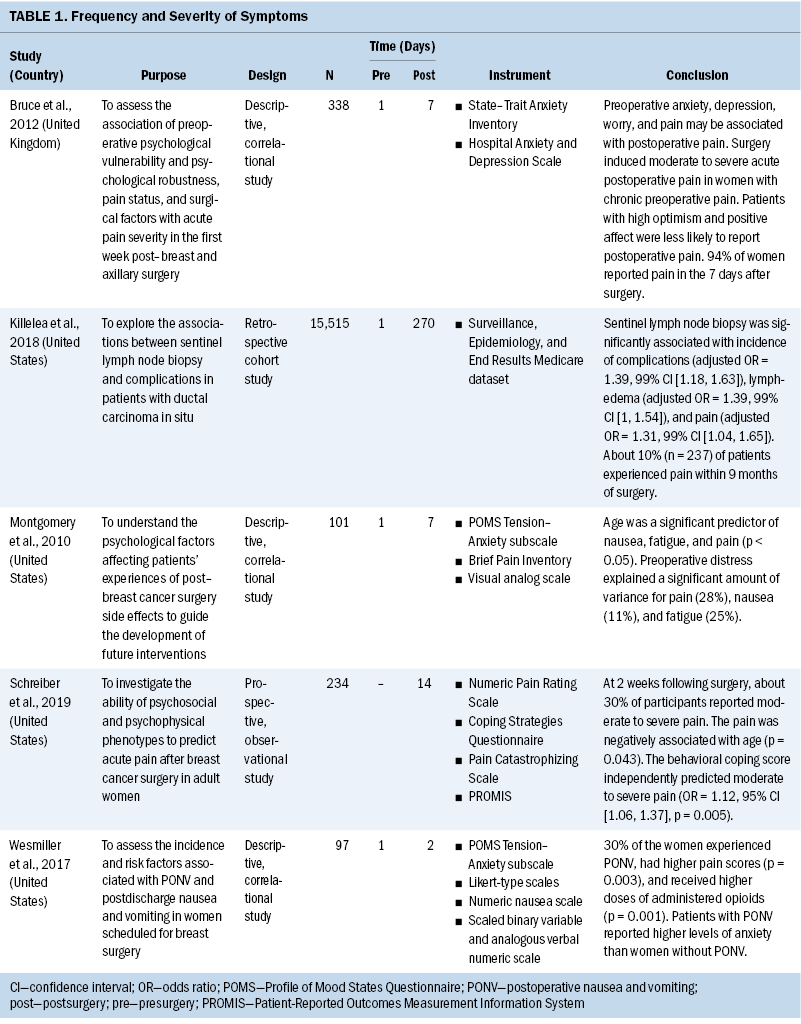
The findings suggest that nausea and pain are substantial problems for women in the early period following breast cancer surgery. Wesmiller et al. (2017) assessed the incidence and risk factors associated with PONV and postdischarge nausea and vomiting in women scheduled for breast surgery from the preoperative period to 48 hours after surgery. The researchers used a prospective comparative design to compare women experiencing nausea and vomiting after surgery with those not experiencing nausea and vomiting after surgery (Wesmiller et al., 2017). The results are consistent with those reported by other researchers and support relationships among pain, opioid administration, and PONV. The study included a small number of women at a single institution. Overall, 30% of the women experienced nausea, and women with PONV had significantly higher verbal pain scores (p = 0.003) and higher anxiety scores as measured by the Profile of Mood States–Short Form (p = 0.08). The findings reveal that participants experienced moderate pain, and 30% of participants experienced nausea 48 hours after surgery. The results illustrate the problem of pain and nausea following breast cancer surgery; however, the researchers did not collect data on postoperative psychological symptoms.
In one of the most robust investigations, Schreiber et al. (2019) investigated the ability of psychosocial and psychophysical phenotypes to predict acute pain after breast cancer surgery in adult women (N = 234). Adult female patients scheduled to undergo breast-conserving surgery or total mastectomy were recruited during their preoperative evaluations. About 30% of the patients approached declined to participate; the most common reason cited was feeling overwhelmed and anxious about the upcoming surgery, which potentially biased the sample toward less catastrophizing and less anxious patients. Although the authors collected data regarding lymph node involvement and pain within 24 hours of surgery, they did not include them in their analysis. The authors concluded that individuals with certain phenotypic characteristics (including older age, lower education level, higher baseline severity and opioid use, and behavioral coping style) were at greater risk for acute pain and opioid use, supporting the need to further explore the relationship between predictors and acute postoperative pain in women undergoing breast cancer surgery.
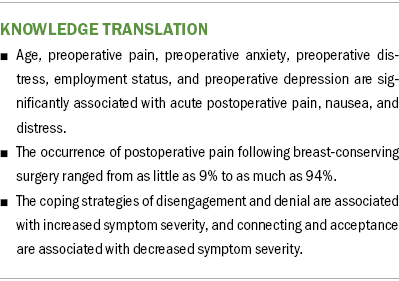
However, differences in study design reduce the strength of this conclusion. The frequency of postoperative pain following breast-conserving therapy ranged from as little as 9% to as much as 94% (Bruce et al., 2012; Killelea et al., 2018; Schreiber et al., 2019). Researchers did not consistently collect or report data from the 24 hours following surgery. The reported rate of nausea in this population was as high as 30% during the postoperative period (Wesmiller et al., 2017). The findings reported by researchers support the existence of a relationship between preoperative and postoperative pain, but researchers have not reported data on the trajectory of distress throughout the initial treatment and surgical period. In addition, although existing literature supports the presence of preoperative anxiety and depression and their relationship with postoperative pain, there are significant gaps in the literature related to the frequency of postoperative distress and quantitative assessment of psychological outcomes, supporting the need for the current review and a clearer understanding of the frequency, severity, and trajectory of pain and distress throughout the initial treatment and surgical period.
Relationships Among Predictors, Pain, Nausea, and Distress
This section discusses the relationships among predictors, pain, nausea, and distress in women undergoing breast cancer surgery. The discussion chronologically presents foundational research before the most recent literature on each subject (see Table 2).
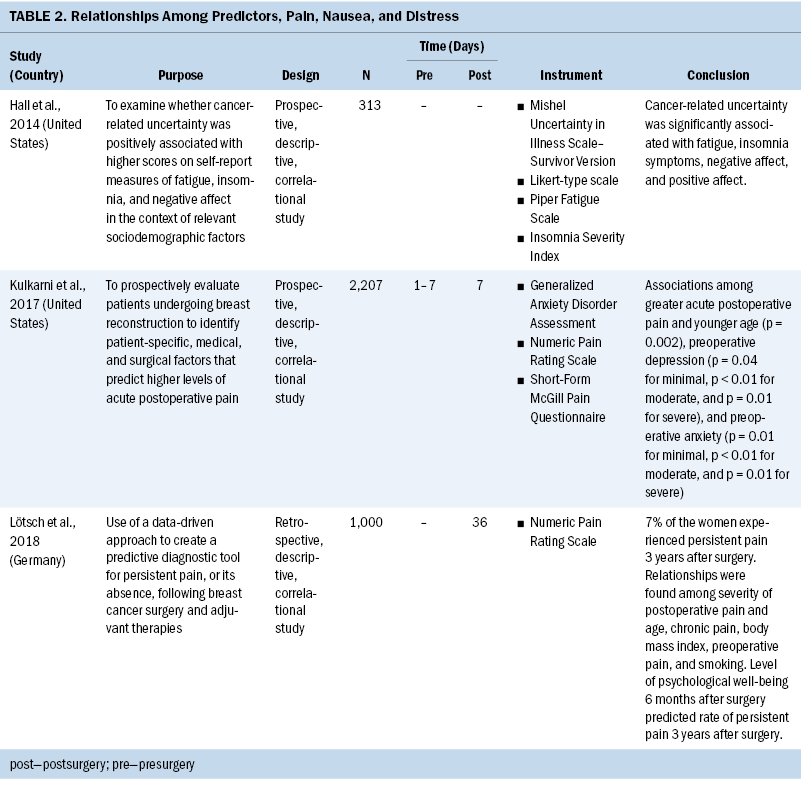
In a large prospective multicenter study, Kulkarni et al. (2017) examined patients undergoing breast reconstruction surgery for breast cancer (N = 2,207). They focused on the value of patient-specific, medical, and surgical factors for predicting the level of acute pain. Although the researchers did not focus on breast-conserving surgery, the similarities between the surgical procedure and the population of their study were relevant to this scoping review in identifying predictors for increased postoperative pain. The strengths of the study include its prospective methodology and study design. The authors used a large sample (N = 2,207, with an 83% response rate) drawn from multiple locations and various surgeons. In addition, the authors used valid and standardized measurement tools. The study also included a well-described, strong statistical analysis. However, the study did have some limitations, including variations in the preoperative survey assessment of patient anxiety and depression symptoms. Other shortcomings of the study included (a) reliance on a sample that was 87% White, making generalizability to other racial or ethnic groups difficult; (b) lack of standardization of postoperative prescriptions for pain across surgeons and institutions, which may have affected self-reported pain experiences; and (c) inconsistency in the time frame for the administration of the preoperative assessment, which patients received one to seven days before surgery. Inconsistency of preoperative assessments may have biased the results.
In addition, some patients may have completed the assessment shortly after receiving their cancer diagnoses, but other patients may have completed it weeks or even months after their initial diagnoses. The preoperative assessment of anxiety, depression, and pain of participants who had just received their diagnoses may have been influenced by their reactions to their diagnoses. Although 83% of patients approached participated in the study, the researchers had no data on those who did not respond and how they differed from the sample.
Overall, Kulkarni et al. (2017) concluded that younger age (p = 0.002), bilateral procedures (p < 0.0001), higher preoperative pain (p < 0.0001), preoperative anxiety (minimal to mild, p = 0.01; moderate, p < 0.01; severe, p = 0.01), and preoperative depression (minimal, p = 0.04; mild to moderate, p < 0.01; moderate to severe, p < 0.01; severe, p = 0.01) were associated with greater acute postoperative pain in women undergoing breast reconstruction surgery. The findings of this study have important implications for the identification of women at risk for significant early postoperative pain following breast reconstruction, which may have longer-term impacts because acute postoperative pain is associated with poor functional outcomes, diminished quality of life, and a greater risk of persistent postsurgical pain (Kulkarni et al., 2017).
Although findings reported in existing literature support relationships among predictors, pain, nausea, and distress, the direction and strength of these relationships are not always clear. Researchers have concluded that age, preoperative pain, preoperative anxiety, preoperative distress, employment status, and preoperative depression are significantly associated with acute postoperative pain, nausea, and distress (Alves et al., 2013; Bruce et al., 2012; Kulkarni et al., 2017; Lötsch et al., 2018; Majumdar et al., 2019). However, researchers have not evaluated these variables consistently. Researchers have also reported relationships among pain, nausea, and distress during the postoperative period; however, significant gaps exist in the literature regarding the relationships among these symptoms from the time a patient undergoes surgery to the time the patient finds out pathology results. Therefore, it is essential to investigate the direction and strength of the relationships between symptoms and predictors in this time frame.
Relationships Among Coping Strategies, Pain, Nausea, and Distress
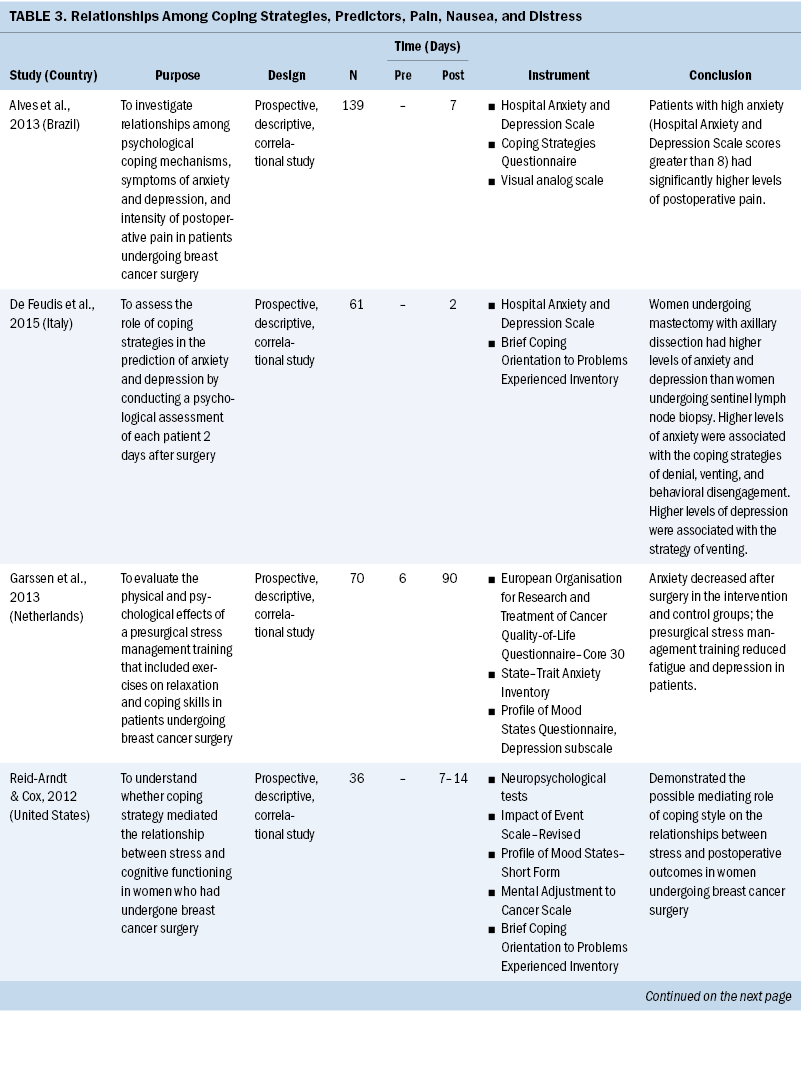
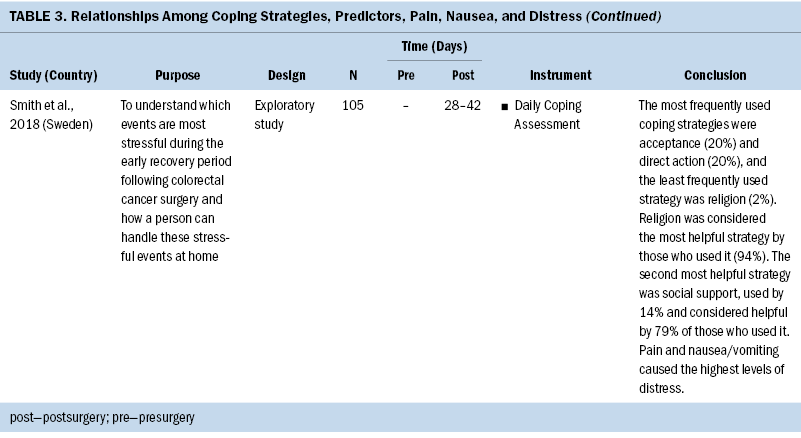
This section reviews the work of researchers who have explored the relationships among coping strategies, pain, nausea, and distress in patients undergoing breast cancer surgery (see Table 3). De Feudis et al. (2015) conducted a descriptive, correlational study investigating the role of coping strategies in predicting emotional distress in patients, comparing women undergoing a sentinel lymph node biopsy with breast-conserving surgery with women undergoing mastectomy and axillary dissection (N = 61). The authors examined the role of coping strategies in predicting anxiety and depression by conducting a psychological assessment of each patient two days after surgery. The assessment consisted of a semistructured interview followed by administration of the Hospital Anxiety and Depression Scale and the Brief Coping Orientation to Problems Experienced Inventory. The results indicated that women undergoing mastectomy with axillary dissection experienced higher levels of anxiety and depression than women undergoing sentinel lymph node biopsy. Higher levels of anxiety were also associated with the dysfunctional and avoidant coping strategies of denial, venting, and behavioral disengagement, and higher levels of depression were associated with the strategy of venting.
Discussion
This scoping review presented the results of 13 peer-reviewed studies that investigated the symptoms and coping strategies experienced by women undergoing breast-conserving surgery for cancer. Specifically, the review identified the frequency and severity of symptoms; the predictors for severe pain, nausea, and distress in this population; and the relationships between coping strategies and these symptoms.
First, this review found that women experience symptoms of pain, nausea, and distress following breast cancer surgery. However, there was a notable lack of consistency in design and results regarding the frequency of pain and distress throughout the perioperative period. In fact, the frequency of postoperative pain following breast-conserving therapy ranged from as low as 9% to as high as 94% (Bruce et al., 2012; Killelea et al., 2018; Schreiber et al., 2019). In addition, researchers ignored the acute postoperative period and did not consistently collect or report data on postoperative day 1. Also, although the literature identified preoperative anxiety and depression as potential problems in this population, the frequency of postoperative distress and the quantitative assessment of psychological symptoms postoperatively were almost completely absent. The substantial gaps in the literature support the need to gain a clearer understanding of the frequency, severity, and trajectory of pain and distress during the postoperative recovery period for women undergoing surgery for breast cancer.
Second, this review identified predictors for symptom severity in this study population. Although findings reported in existing literature support relationships among predictors, pain, nausea, and distress, the direction and strength of these relationships are not clear. Researchers have concluded that age, preoperative pain, preoperative anxiety, preoperative distress, employment status, and preoperative depression are significantly associated with acute postoperative pain, nausea, and distress. However, the study designs used by researchers have limited the conclusions possible, justifying the need for further studies to better understand the relationships between variables and outcomes. In addition, there are significant gaps in the literature regarding relationships among these symptoms between the time a patient has surgery and the time the patient receives pathology results. Therefore, based on existing literature, further investigation of the direction and the strength of relationships among these variables in this time frame is warranted.
Third, this review presented the literature about the relationships between coping strategies and symptom severity in women undergoing breast-conserving surgery. The findings reported in existing literature indicate the magnitude of the coping resources required in this population. In particular, the literature associated disengagement and denial with increased symptom severity and connected acceptance with decreased symptom severity. In addition, those findings support the possible mediating role of coping style on the relationship between predictors and symptom severity within this population. However, the relationships among coping strategies, symptom severity, and predictors within this population remains unknown. Overall, this review captured emerging knowledge, identified where scientific advancement is required, and assisted with the development of future interventions to address these symptoms.
Implications for Nursing
Identifying the frequency and severity of symptoms can be useful for oncology nurses and patients to set appropriate expectations. Even the reassurance that a symptom such as preoperative distress is common can provide comfort. In addition, many patients may be expecting little or no pain 24 hours or two weeks following surgery, but describing the incidence ahead of the surgical period can help them set proper expectations for their recovery and help in their planning for the recovery period.
This scoping review demonstrates additional areas for improving the implementation of evidence-based interventions to manage untreated pain, nausea, and distress. Most patients do not see their surgeons for follow-up until several weeks after surgery, when many symptoms may have already resolved themselves; however, self-resolution of symptoms does not decrease the suffering of patients during the period before follow-up, which may increase anxiety related to unmanaged symptoms for future surgeries.
Conclusion
As the frequency of surgeries performed on an outpatient basis continues to increase, oncology nurses need to assess and treat symptoms outside the hospital setting. This scoping review demonstrated that nausea, pain, and distress are substantial problems for women following breast cancer surgery. The literature supports the existence of relationships among predictors, pain, nausea, and distress. However, the direction and strength of these relationships are not clear. An improved understanding of the relationships among these factors is important to improve the experience of women with breast cancer. Therefore, future nursing research should focus on improving the understanding of these relationships and developing targeted interventions to reduce these symptoms.
About the Authors
Jennifer Ross Majumdar, PhD, MSN, CRNA, is a nurse scientist in the Department of Nursing at Memorial Sloan Kettering Cancer Center in New York, NY, and adjunct assistant professor in the Hunter-Bellevue School of Nursing at Hunter College at the City University of New York; and Stephen J. Yermal, PhD, RN, CRNA, is the William Randolph Hearst Endowed Chair in Clinical Nursing and the associate dean for graduate programs in the Hunter-Bellevue School of Nursing at Hunter College at the City University of New York. This research was supported, in part, by the National Institutes of Health and National Cancer Institute with a Cancer Center Support Grant to Memorial Sloan Kettering Cancer Center (P30 CA008748). Majumdar completed the data collection and provided statistical support and the analysis. Both authors contributed to the conceptualization and design and the manuscript preparation. Majumdar can be reached at rossj2@mskcc.org, with copy to ONFEditor@ons.org. (Submitted March 2023. Accepted October 24, 2023.)
References
Alves, M.L., Vieira, J.E., Mathias, L.A.S.T., & Gozzani, J.L. (2013). Preoperative coping mechanisms have no predictive value for postoperative pain in breast cancer. Revista Brasileira de Psiquiatria, 35(4), 364–368. https://doi.org/10.1590/1516-4446-2012-0934
Arksey, H., & O’Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. https://doi.org/10.1080/1364557032000119616
Bruce, J., Thornton, A.J., Scott, N.W., Marfizo, S., Powell, R., Johnston, M., . . . Thompson, A.M. (2012). Chronic preoperative pain and psychological robustness predict acute postoperative pain outcomes after surgery for breast cancer. British Journal of Cancer, 107(6), 937–946. https://doi.org/10.1038/bjc.2012.341
Chatterjee, A., Pyfer, B., Czerniecki, B., Rosenkranz, K., Tchou, J., & Fisher, C. (2015). Early postoperative outcomes in lumpectomy versus simple mastectomy. Journal of Surgical Research, 198(1), 143–148. https://doi.org/10.1016/j.jss.2015.01.054
De Feudis, R., Lanciano, T., & Rinaldi, S. (2015). Coping strategies of southern Italian women predict distress following breast cancer surgery. Europe’s Journal of Psychology, 11(2), 280–294. https://doi.org/10.5964/ejop.v11i2.908
DeSantis, C.E., Ma, J., Gaudet, M.M., Newman, L.A., Miller, K.D., Goding Sauer, A., . . . Siegel, R.L. (2019). Breast cancer statistics, 2019. CA: A Cancer Journal for Clinicians, 69(6), 438–451. https://doi.org/10.3322/caac.21583
Garssen, B., Boomsma, M.F., de Jager Meezenbroek, E., Porsild, T., Berkhof, J., Berbee, M., . . . Beelen, R.H.J. (2013). Stress management training for breast cancer surgery patients. Psycho-Oncology, 22(3), 572–580. https://doi.org/10.1002/pon.3034
Giaquinto, A.N., Sung, H., Miller, K.D., Kramer, J.L., Newman, L.A., Minihan, A., . . . Siegel, R.L. (2022). Breast cancer statistics, 2022. CA: A Cancer Journal for Clinicians, 72(6), 524–541. https://doi.org/10.3322/caac.21754
Hall, D.L., Mishel, M.H., & Germino, B.B. (2014). Living with cancer-related uncertainty: Associations with fatigue, insomnia, and affect in younger breast cancer survivors. Supportive Care in Cancer, 22(9), 2489–2495. https://doi.org/10.1007/s00520-014-2243-y
Hartmann-Johnsen, O.J., Kåresen, R., Schlichting, E., & Nygård, J.F. (2015). Survival is better after breast conserving therapy than mastectomy for early stage breast cancer: A registry-based follow-up study of Norwegian women primary operated between 1998 and 2008. Annals of Surgical Oncology, 22(12), 3836–3845. https://doi.org/10.1245/s10434-015-4441-3
Hwang, E.S., Lichtensztajn, D.Y., Gomez, S.L., Fowble, B., & Clarke, C.A. (2013). Survival after lumpectomy and mastectomy for early stage invasive breast cancer. Cancer, 119(7), 1402–1411. https://doi.org/10.1002/cncr.27795
Killelea, B.K., Long, J.B., Dang, W., Mougalian, S.S., Evans, S.B., Gross, C.P., & Wang, S.-Y. (2018). Associations between sentinel lymph node biopsy and complications for patients with ductal carcinoma in situ. Annals of Surgical Oncology, 25(6), 1521–1529. https://doi.org/10.1245/s10434-018-6410-0
Kulkarni, A.R., Pusic, A.L., Hamill, J.B., Kim, H.M., Qi, J., Wilkins, E.G., & Roth, R.S. (2017). Factors associated with acute postoperative pain following breast reconstruction. JPRAS Open, 11, 1–13. https://doi.org/10.1016/j.jpra.2016.08.005
Lötsch, J., Sipilä, R., Tasmuth, T., Kringel, D., Estlander, A.-M., Meretoja, T., . . . Ultsch, A. (2018). Machine-learning-derived classifier predicts absence of persistent pain after breast cancer surgery with high accuracy. Breast Cancer Research and Treatment, 171(2), 399–411. https://doi.org/10.1007/S10549-018-4841-8
Majumdar, J.R., Assel, M.J., Lang, S.A., Vickers, A.J., & Afonso, A.M. (2022). Implementation of an enhanced recovery protocol in patients undergoing mastectomies for breast cancer: An interrupted time-series design. Asia-Pacific Journal of Oncology Nursing, 9(7), 100047. https://doi.org/10.1016/J.APJON.2022.02.009
Majumdar, J.R., Vertosick, E., Assel, M., Soeprono, M., Groeger, H., Marte, M.K., . . . Twersky, R. (2021). Reduction of postoperative nausea and vomiting and unplanned extended stays in outpatient plastic surgeries with a standardized protocol. Journal of Clinical Anesthesia, 74, 110419. https://doi.org/10.1016/J.JCLINANE.2021.110419
Majumdar, J.R., Vertosick, E.A., Cohen, B., Assel, M., Levine, M., & Barton-Burke, M. (2019). Preoperative anxiety in patients undergoing outpatient cancer surgery. Asia-Pacific Journal of Oncology Nursing, 6(4), 440–445. https://doi.org/10.4103/apjon.apjon_16_19
Montgomery, G.H., Schnur, J.B., Erblich, J., Diefenbach, M.A., & Bovbjerg, D.H. (2010). Presurgery psychological factors predict pain, nausea, and fatigue one week after breast cancer surgery. Journal of Pain and Symptom Management, 39(6), 1043–1052. https://doi.org/10.1016/j.jpainsymman.2009.11.318
National Comprehensive Cancer Network. (2023). NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): Distress management [v.2.2023]. https://www.nccn.org/professionals/physician_gls/pdf/distress.pdf
Reid-Arndt, S.A., & Cox, C.R. (2012). Stress, coping and cognitive deficits in women after surgery for breast cancer. Journal of Clinical Psychology in Medical Settings, 19(2), 127–137. https://doi.org/10.1007/s10880-011-9274-z
Schreiber, K.L., Zinboonyahgoon, N., Xu, X., Spivey, T., King, T., Dominici, L., . . . Edwards, R.R. (2019). Preoperative psychosocial and psychophysical phenotypes as predictors of acute pain outcomes after breast surgery. Journal of Pain, 20(5), 540–556. https://doi.org/10.1016/j.jpain.2018.11.004
Siegel, R.L., Miller, K.D., Wagle, N.S., & Jemal, A. (2023). Cancer statistics, 2023. CA: A Cancer Journal for Clinicians, 73(1), 17–48. https://doi.org/10.3322/caac.21763
Smith, F., Öhlén, J., Persson, L.-O., & Carlsson, E. (2018). Daily assessment of stressful events and coping in early post-operative recovery after colorectal cancer surgery. European Journal of Cancer Care, 27(2), e12829. https://doi.org/10.1111/ecc.12829
Wesmiller, S.W., Bender, C.M., Conley, Y.P., Bovbjerg, D.H., Ahrendt, G., Bonaventura, M., & Sereika, S.M. (2017). A prospective study of nausea and vomiting after breast cancer surgery. Journal of PeriAnesthesia Nursing, 32(3), 169–176. https://doi.org/10.1016/j.jopan.2015.12.009



