Factors Associated With Post-Traumatic Growth, Quality of Life, and Spiritual Well-Being in Outpatients Undergoing Bone Marrow Transplantation: A Pilot Study
Purpose/Objectives: To examine the relationships between spiritual, religious, and sociodemographic factors and post-traumatic growth, quality of life, and spiritual well-being in outpatients undergoing bone marrow and/or stem cell transplantation (BMSCT).
Design: Cross-sectional, descriptive, exploratory.
Setting: Outpatient bone marrow transplantation clinic at the Tom Baker Cancer Centre in Calgary, Alberta, Canada.
Sample: 100 patients (21 pre-BMSCT and 79 post-BMSCT) accrued consecutively via non-probability sampling.
Methods: Study participants completed the Functional Assessment of Cancer Therapy–Bone Marrow Transplantation (FACT-BMT), the Post-Traumatic Growth Inventory (PTGI), the Functional Assessment of Chronic Illness Therapy–Spiritual Well-Being (FACIT-Sp), and a demographic questionnaire. Data analysis included descriptive statistics, t tests, and correlational analyses.
Main Research Variables: Demographic variables, FACT-BMT scores, PTGI scores, FACIT-Sp scores.
Findings: The majority of participants identified themselves as being at least somewhat spiritual. Significant differences were noted between those who identified as being not religious at all versus having at least some religiosity in several subscales of the PTGI, as well as on the FACIT-Sp. Similarly, significant differences were observed between participants who identified as being not spiritual at all versus having at least some spirituality for several subscales on the PTGI. Most participants indicated they would be at least somewhat likely to recommend spiritual care to a new patient.
Conclusions: Most patients in this study within a publicly funded healthcare system self-identified with spirituality, used spiritual resources, and would recommend that other patients undergoing BMSCT seek the support of a spiritual care professional or chaplain. Spirituality, along with practical and relational factors, had a positive impact on certain aspects of post-traumatic growth, quality of life, and spiritual and physical well-being.
Implications for Nursing: Oncology nurses are encouraged to routinely address spiritual issues. Findings from this study suggest that spirituality is not only important to patients undergoing BMSCT, but also may be an integral component of patients’ post-traumatic growth, quality of life, and spiritual well-being.
Jump to a section
Being diagnosed with and treated for blood and/or bone marrow cancer affects patients’ quality of life, including their physical, psychosocial, and spiritual well-being (Andrykowski et al., 2005; Ferrell et al., 1992; Pidala, Anasetti, & Jim, 2009; Saleh & Brockopp, 2001). Quality of life in cancer populations refers to the appraisal and evaluation of a patient’s actual functional status across various domains of health in comparison to the functional status he or she expects or desires (Calman, 1984; Cella & Tulsky, 1993). Pragmatically, quality of life has been conceptualized as an equation: Quality of life equals reality minus expectations (Calman, 1984). However, the clinical ramifications related to the nature and impact of these issues are complex and dynamic, and they have a significant effect on health outcomes and patients’ ability to cope (Andrykowski et al., 2005; Ferrell et al., 1992; Pidala et al., 2009; Sirilla & Overcash, 2012; Whedon & Ferrell, 1994). Research has primarily focused on the significant negative effects that cancer and its treatment have on aspects of physical well-being (Andrykowski et al., 2005; Pidala et al., 2009), whereas the psychosocial and spiritual domains remain underresearched and underaddressed clinically (Kristeller, Zumbrun, & Schilling, 1999; Zabora, BrintzenhofeSzoc, Curbow, Hooker, & Piantadosi, 2001), often being relegated in clinical practice to an ancillary service (Kristeller et al., 1999; Sinclair & Chochinov, 2012a, 2012b; Sinclair, Mysak, & Hagen, 2009). The aim of this cross-sectional pilot study was to explore the relationships between spiritual, religious, and sociodemographic factors and post-traumatic growth, quality of life, and spiritual well-being in outpatient patients undergoing bone marrow and/or stem cell transplantation (BMSCT).
Literature Review
Research on quality of life within the BMSCT population has primarily focused on the impact of disease and treatment on aspects of physical well-being (Pidala et al., 2009). This is partially because symptom burden often involves treatment-related toxicities, graft-versus-host disease, gastrointestinal issues, reduced mobility, fatigue, and effects on sexuality, most of which gradually improve over time (Le et al., 2010). The impact of undergoing BMSCT on spiritual well-being and, conversely, the potential buffering effect of spirituality on patients’ quality of life (i.e., spirituality potentially reducing distress associated with poor quality of life) are largely nascent. Although theoretical frameworks (Ferrell et al., 1992) and evidence suggest that spiritual issues are significant and prevalent within the BMSCT population, much of this literature is anecdotal, theoretical, and/or dialogical in nature (Berger, 2001; Cohen, Headley, & Sherwood, 2000; King & Crisp, 2007).
The small number of empirical studies exploring the relationship between spiritual well-being and other facets of quality of life of patients undergoing BMSCT have produced largely mixed results (Pidala et al., 2009). Sirilla and Overcash (2012) reported that spiritual well-being increased as time lapsed from transplantation, whereas Andrykowski et al. (2005) observed poorer spiritual well-being among transplantation survivors over time (study participants were, on average, seven-year survivors). Spirituality, particularly its meaning and peace dimensions (Peterman, Fitchett, Brady, Hernandez, & Cella, 2002), seems to have a buffering effect on end-of-life distress (Sinclair & Chochinov, 2012c) and is one of the most important and frequently used coping resources by patients with cancer (Sirilla & Overcash, 2012; Zaza, Sellick, & Hillier, 2005). A study of newly diagnosed patients with cancer reported that the meaning and peace dimension of spirituality, versus the faith dimension that had no significant effect, predicted quality of life (Whitford & Olver, 2012). Likewise, religious and spiritual coping has been reported to have a positive effect on post-traumatic growth in patients with cervical cancer (Smith, Dalen, Bernard, & Baumgartner, 2008), breast cancer survivors (Carpenter, Brockopp, & Andrykowski, 1999; Lelorain, Bonnaud-Antignac, & Florin, 2010), and family caregivers of patients with cancer in India (Thombre, Sherman, & Simonton, 2010). Conversely, religious and spiritual struggle is recognized as a prominent issue in long-term hematopoietic stem cell transplantation survivors and is associated with greater depression and poorer quality of life (King et al., 2015). Despite patients with cancer reporting that their spiritual well-being was affected by and helped them cope with their illness, these issues are often not addressed or documented in the patient chart (Alcorn et al., 2010; Balboni et al., 2007; King & Crisp, 2007).
A study involving 200 oncologists and 113 oncology nurses indicated that most desire to provide spiritual care (74% versus 60%, respectively, p = 0.002), with 41% of oncologists and 39% of oncology nurses indicating that they provide spiritual care less often than they desire, citing a lack of time and private space, as well as inadequate training, as the highest ranking barriers (Balboni et al., 2014). The discord between the purported importance of addressing spiritual needs by oncology nurses (85%, n = 97) and their ability to address these needs is considerable, with only 12 of 48 patient participants reporting to have received spiritual care across the cancer trajectory (Phelps et al., 2012). Similarly, although about 48% (n = 127) of 267 oncology nurses identified themselves as being primarily responsible for addressing patient spiritual distress, only about 9% of nurses ranked addressing spiritual distress as a priority when caring for patients with a poor prognosis compared with 17 other psychosocial issues (Kristeller et al., 1999). The lack of research and mixed results seem to be attributable to the ephemeral nature of the research topic and the challenge of addressing these issues in a clinical setting (Sinclair & Chochinov, 2012a, 2012b). In this study, spirituality is defined as “an individual’s beliefs, values, behaviours and experiences related to ultimate meaning” (Sinclair & Chochinov, 2012b, p. 260).
Although studies on the spiritual and psychosocial aspects of quality of life in patients undergoing BMSCT have begun to emerge (Andrykowski et al., 2005; King et al., 2015; Sirilla & Overcash, 2012; Widows, Jacobsen, Booth-Jones, & Fields, 2005), the current study extends this research in a number of ways. This study focuses on patients across the treatment continuum, from diagnosis to survivorship and palliative care, rather than at a given time point or stage. In addition, it examines, in detail, the relationships between religious and spiritual demographic variables and facets of quality of life. As a subset of a mixed-methods study, these data provide a snapshot into the experiential world of patients undergoing BMSCT, which, when combined with qualitative data (Sinclair et al., 2015), provides an empirically based approach to spiritual care delivery that is clinically informed and relevant.
Methods
This study was part of a larger mixed-methods study that inquired into the quality of life and spiritual well-being of patients undergoing BMSCT and how to address these issues within an interdisciplinary clinical team (Sinclair et al., 2015). This article reports on the results of a cross-sectional survey of patients undergoing BMSCT that was conducted in a BMSCT clinic housed within the Tom Baker Cancer Centre, a large outpatient cancer center in Calgary, Alberta, Canada. Data collection commenced in December 2012 and was completed in June 2013. Ethics approval was granted by the Conjoint Health Research Ethics Board at the University of Calgary, and permission to contact and access patients was granted by the cancer care center.
Participants and Procedure
Participants were patients engaged in the outpatient BMSCT clinic within a large urban cancer care center. The inclusion criteria for patients were as follows: being aged 18 years or older, being able to speak and read English, being a patient within the BMSCT clinic, having no evidence of dementia or delirium (as determined by clinical staff, including nurses, physicians, and allied health professionals), and being willing to provide written informed consent. Participants were initially identified by clinical staff and given a brief description of the study; if interested, they were provided with more details about the study by the research coordinator, who also determined eligibility. If the participants were deemed eligible, written informed consent and basic demographic information were collected. Participants were given the three study measures, which were self-administered during a routine clinical visit. Completed surveys were placed in a sealed envelope and given to a research assistant for data entry.
Measures
Three measures were used to assess participants’ overall quality of life, post-traumatic growth, and spiritual well-being: the Functional Assessment of Cancer Therapy–Bone Marrow Transplantation (FACT-BMT) (McQuellon et al., 1997), the Post-Traumatic Growth Inventory (PTGI) (Tedeschi & Calhoun, 1996), and the Functional Assessment of Chronic Illness Therapy–Spiritual Well-Being (FACIT-Sp) (Peterman et al., 2002). The 47-item FACT-BMT is a valid and reliable measure of five dimensions of quality of life in patients undergoing bone marrow transplantation: physical well-being, social and family well-being, emotional well-being, functional well-being, and additional concerns. The PTGI is a validated 21-item inventory designed to measure positive changes associated with a cancer diagnosis consisting of five factors: relating to others, new possibilities, personal strength, spiritual change, and appreciation of life. The FACIT-Sp is a 12-item, psychometrically sound measure of spiritual well-being consisting of two subscales: sense of meaning and peace, and role of faith in illness. In addition to the three measures, patients were administered a demographic questionnaire.
Results
Sample
The majority of the 100 patients had undergone (n = 75) or were awaiting (n = 4) allogeneic BMSCT; 10 patients had undergone autologous BMSCT, and 12 were awaiting autologous BMSCT. One patient had undergone autologous BMSCT and was proceeding to allogeneic BMSCT. Of those participants who had undergone transplantation, the mean time since transplantation was 3.85 years (1,404 days), with a range of 3–10,868 days (29.77 years). Additional demographic information is summarized in Table 1.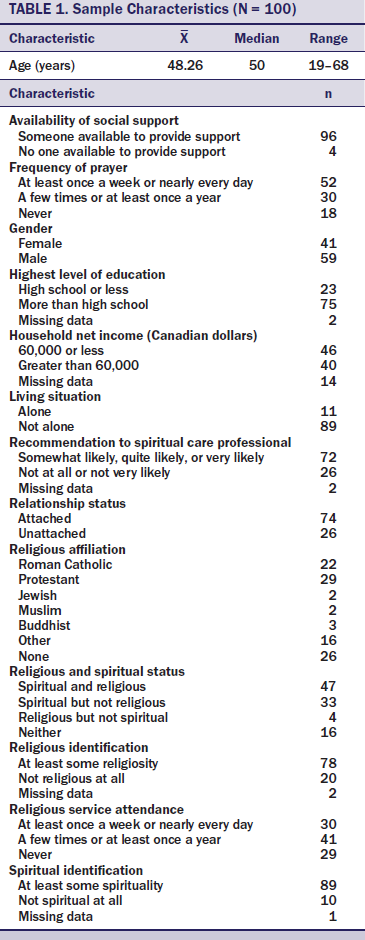
Correlations
Pearson’s r was calculated to look for significant relationships among demographic variables and the overall results of the FACT-BMT, PTGI, and FACIT-Sp. No significant relationships were found among age or marital status and any of the scores from the FACT-BMT, PTGI, and FACIT-Sp. In addition, no significant relationships were noted between time since transplantation and results of the FACT-BMT and PTGI. No significant relationships were observed between type of transplantation (allogeneic versus autologous) and any of the results of the measures.
T Tests
T tests were performed to look for relevant differences in the FACT-BMT, PTGI, and FACIT-Sp scores between groups, as determined by various demographic variables. Statistically significant differences were found between participants who identified themselves as being attached versus unattached only for the first item on the PTGI (relating to others) (t[96] = 2.21, p = 0.029). Similarly, differences were discovered on the first item of the PTGI for participants who identified that they lived alone versus not alone (t[96] = –2.874, p = 0.005). Differences were noted between participants who identified that they had someone versus no one for support, but only for the FACT-BMT physical well-being subscale (p = 0.008). Statistically significant differences were revealed between participants who reported a mean household net income of $60,000 or less and those who reported a mean household net income of greater than $60,000 for the FACIT-Sp meaning subscale (t[84] = –2.301, p = 0.024) and the FACT-BMT spiritual well-being subscale (t[84] = –2.708, p = 0.008). No significant differences were found on any of the measures between participants who identified that they had more than a high school education versus a high school education or less.
T tests were used to look for differences in responses on the FACT-BMT, PTGI, and FACIT-Sp between participants who identified as being not religious at all versus having at least some religiosity, as well as between participants who identified as being not spiritual at all versus having at least some spirituality (see Table 2). Significant differences were observed between those who identified as being not religious at all versus having at least some religiosity in several subscales of the PTGI (relating to others, new possibilities, personal strength, spiritual change, appreciation of life, and PTGI all [the total for all subscales of the PTGI]) and on the FACIT-Sp (faith subscale and total score). Similarly, significant differences were noted between participants who identified as being not spiritual at all versus having at least some spirituality for several subscales on the PTGI (relating to others, new possibilities, personal strength, spiritual change, appreciation of life, and the total score for all PTGI subscales). No statistically significant differences were found among those who identified as being not religious (or spiritual) at all versus having at least some religiosity (or spirituality) on any of the subscales or total score of the FACT-BMT. 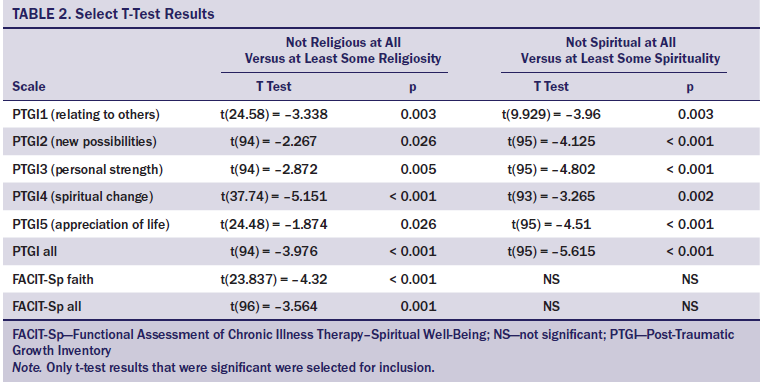
Individual Item Responses
When individual item responses on the various measures were examined, several findings emerged. Notable results from the FACT-BMT included the finding that 84 of 94 respondents did not regret having a transplantation, whereas only 4 respondents regretted having the transplantation very much. Just 2 of 99 respondents indicated that they were not at all able to enjoy life, whereas 71 indicated they were able to enjoy life either quite a bit (n = 41) or very much (n = 30). Ninety-seven of 98 respondents indicated that they were not at all (n = 82) or a little bit (n = 13) concerned they were losing hope in their fight against their illness, with only 3 respondents indicating they were at least somewhat concerned (n = 2; one respondent was quite a bit concerned). Eight of 99 respondents were not at all content with their current quality of life, and 91 were at least a little bit content with their current quality of life (n = 11; 30 were somewhat content, 34 were quite a bit content, and 16 were very much content). Forty-five of 96 respondents were at least somewhat concerned that their illness was a personal hardship for close family members.
In terms of individual religious and spiritual item responses, 59 of the 74 respondents who identified a religious affiliation were at least somewhat likely to recommend that a new patient seek the support of the clinic’s spiritual care professional (chaplain), with only 3 being not at all likely to recommend spiritual care support. Among respondents who did not identify a religious affiliation (n = 26), n = 13 were at least somewhat likely to recommend that a new patient seek the support of the clinics spiritual care professional. Twenty-three respondents who identified themselves as spiritual but not religious (n = 33) were at least somewhat likely to recommend spiritual care to a new patient, whereas 5 patients who indicated they were neither spiritual nor religious (n = 16) were at least somewhat likely to recommend spiritual care.
Discussion
Understanding and addressing issues related to quality of life are recognized as key aspects of integrated person-centered cancer care (Andrykowski et al., 2005; Ferrell et al., 1992; Fromm, Andrykowski, & Hunt, 1996; Gaston-Johansson & Foxall, 1996; Whedon & Ferrell, 1994; World Health Organization, 2015). This cross-sectional pilot study is the first known study to investigate the relationships among post-traumatic growth, quality of life, and spiritual well-being in patients at various time points across the BMSCT cancer trajectory ranging from diagnosis to survivorship and palliative care.
Impact on Aspects of Quality of Life
A BMSCT is one of the most challenging forms of cancer treatment, and it affects patient quality of life and healthcare provider moral distress related to treatment burden versus benefit. Remarkably, study participants who had undergone a transplantation indicated that they did not regret doing so, were highly hopeful, and were at least a little bit content with their quality of life, suggesting that quality of life fluctuates and is relative to life circumstances. Seventy-nine of 100 study participants underwent allogeneic transplantation, and the average time since transplantation was about three years; these factors may have contributed to the lack of a significant relationship between the type of transplantation and the overall results of the measures. The high degree of satisfaction associated with patient quality of life seemed to confirm the Calman (1984) gap hypothesis of quality of life in patients with cancer (quality of life equals reality minus expectations). In relation to this study, the expectations of patients undergoing BMSCT and their understanding of the reality of their situation were more closely aligned than healthy individuals’ estimates—and perhaps more than the patients themselves estimated prior to diagnosis and treatment (Byar, Eilers, & Nuss, 2005; Ubel, Loewenstein, & Jepson, 2003). This may be attributable, in part, to the current study’s outpatient sample; outpatients typically report a much higher quality of life compared to inpatients who, by virtue of being admitted, have more acute symptoms and illness severity, diminishing their quality of life (Reuter, Raugust, Marschner, & Härter, 2007).
Impact on Quality of Life and Spiritual Well-Being
A strong positive effect of marital status on cancer survivorship has been reported, with married patients being more likely to present at an earlier stage, to receive curative treatment, and to survive longer than patients who were single, separated, or divorced across the 10 leading types of cancer (Aizer et al., 2013). As Kissane (2013) noted, “the benefits of marriage are comparable to or greater than anticancer treatment with chemotherapy” (p. 3,852). The current study builds on these findings, suggesting that in relation to quality of life, being in a relationship and cohabiting with another person, whether as a result of marriage, commitment, or a mutually beneficial relationship, seem to be essential underlying factors. Although no statistically significant difference was found between these interpersonal factors and participants being able to identify a supportive person in their life, a statistically significant negative relationship was observed between physical well-being, as measured by the FACT-BMT, and being unable to identify someone as a source of social support. Similarly, within the publicly funded Canadian healthcare system, having a household income of greater than $60,000 had a statistically significant association with higher spiritual well-being (0.008), as measured by the FACT-BMT and the meaning and purpose dimensions (p = 0.024) of the FACIT-Sp.
These findings seem to suggest that practical and relational factors are one of the greatest predictors of physical, social, and spiritual well-being; being accompanied through the cancer trajectory and having more financial resources appears to be a profoundly different experience than navigating the cancer journey alone or with financial concerns. Although household income, relationship status, and living situation may have spiritual correlates, such as a sense of equanimity, belonging, and love, the current authors’ findings also suggest that the effect of addressing these essential basic needs traverses multiple domains of quality of life (Maslow, 1943).
Spirituality and Religion Within the Cancer Journey
Spirituality may have broad applicability and relevance across diverse patient populations because patients seem to primarily identify themselves as spiritual, with religious expressions of spirituality having an important, but secondary, role. These results are consistent with findings indicating a positive relationship between the meaning and peace dimensions of spirituality and patient quality of life versus faith alone, suggesting that the individualized and experiential aspects of spirituality have the greatest impact on quality of life (Whitford & Olver, 2012).
The importance of a routine and broad approach to spiritual care is further supported by research within health care demonstrating an association between spiritual and religious struggle and depression and quality of life (King et al., 2015). The appropriateness and importance of routine spiritual screening is also supported by research within the social sciences indicating that, when spirituality is understood as finding a sense of connection and meaning in life, it is a care domain that is important to even atheists and agnostics (Smith-Stoner, 2007). Study results are also congruent with Canadian and American survey data that reflect an increasing trend within society toward identification with spirituality, coupled with a decline in religiosity (Clark & Schellenberg, 2006; Graduate Center of the City University of New York, 2001). However, although the traditional facets of religiosity (affiliation, attendance, importance, and practice) seem to be declining, intrinsic religiosity as determined by the individual, in contrast to dogma or a religious institution, remains an important and well-used resource. Although patients may not identify themselves as religious on their intake assessment, they may nonetheless have practices, such as prayer, that are significantly important to them. This interpretation is supported by studies within a BMSCT population (Sirilla & Overcash, 2012) and across various cancer populations (Zaza et al., 2005), members of which have identified spiritual and religious practices as some of the most important and well-used coping resources.
In addition to the importance that patients ascribed to spirituality, a positive relationship between certain aspects of quality of life and post-traumatic growth were more likely to be reported in individuals who were religious and spiritual versus those who identified as not being religious or spiritual at all. A statistically significant difference was noted between individuals who were at least somewhat religious compared to those who were not at all religious on four of the five factors of the PTGI (relating to others, new possibilities, personal strength, and spiritual change); this suggests that religion may function as a guide or a framework to not only help patients cope, but also to frame their illness within a larger worldview. Self-identifying as being at least somewhat spiritual had a similar effect on factors of the PTGI, with the exception that no statistically significant difference was noted in relation to the factor of spiritual change, whereas the factor of appreciation for life demonstrated a statistically significant difference. This may suggest that preexisting spirituality is less adaptable to change and that developing an appreciation for life may be more strongly associated with personal experience and convictions than with dogma or externalized religiosity.
Limitations
A number of limitations affect the generalizability of this study’s findings, including limitations inherent to cross-sectional studies (Costantini & Higginson, 2007) (namely, that they do not take into account fluctuations in study variables that are accounted for in longitudinal studies). Therefore, generalizability cannot be assumed within a singular case. Although causation cannot be demonstrated in cross-sectional studies, the relationships between spirituality, post-traumatic growth, and quality of life seem to be implied; however, the nature and strength of these relationships requires additional research and is further complicated by overlapping concepts within and between study measures. By informing patients about the nature of the study prior to obtaining informed consent, a sample bias may have been introduced where a disproportionate number of individuals being recruited had high levels of quality of life, spiritual well-being, and post-traumatic growth.
Although the participation rate (80 of 119 patients who were approached agreed to participate; the participation rate was not collected for the first 20 patients) in this study was acceptable, the authors were unable to determine differences between study participants and those who refused to participate in not collecting information on reasons for refusal; these differences often vary considerably (Costantini & Higginson, 2007). The authors aimed to recruit patients undergoing allogeneic and autologous transplantations across the treatment trajectory, but the majority of patients who signed up for the study were patients undergoing allogenic transplantation within the survivorship phase, which likely was a factor in their relatively high quality of life and minimal regrets related to the transplantation. A related limitation is a potential ceiling effect because of the cross-sectional sample, which did not account for expected differences.
Implications for Nursing and Conclusion
This pilot study describes the relationships between spiritual, religious, and sociodemographic factors and post-traumatic growth, quality of life, and spiritual well-being within a BMSCT outpatient population. Findings suggest that patients undergoing BMSCT, within the publicly funded Canadian healthcare system, strongly identify with spirituality and consider spiritual resources to be an important facet of their cancer journey. Although this cross-sectional pilot study was not intended to demonstrate causation, it identified a number of potential and unexpected relationships that warrant future investigation. This includes the relationship of self-reported spirituality with quality of life and post-traumatic growth. In addition, a relationship seemed to exist between more practical variables (e.g., living situation, relationship status, income) and certain aspects of physical and spiritual well-being.
Oncology nurses working within BMSCT clinics are ideally positioned to provide psychosocial and spiritual support, developing long-standing trusting relationships with patients that aim to address their comprehensive needs. Despite oncology nurses often feeling apprehensive and inadequate in addressing spiritual issues (Balboni et al., 2014; Kristeller et al., 1999; Phelps et al., 2012), most study participants self-identified with spirituality and would recommend the support of a spiritual care professional. This seems to suggest that, although spiritual issues are a sensitive topic for nurses to address, they are highly relevant to patients who largely welcome and want their spiritual issues to be addressed. Study results also suggest that spirituality is not only important to patients, but also may enhance quality of life and enable patients to find meaning in the midst of uncertainty, poor physical well-being, and illness-related trauma. The importance that patients place on having their spiritual needs routinely addressed is consistent with the qualitative data of this mixed-methods study involving patients undergoing BMSCT and their healthcare providers (Sinclair et al., 2015). Although a fear of offending patients was a significant barrier to addressing spiritual needs, according to healthcare provider participants, it was a barrier that patient participants diminished and felt needed to be overcome.
The authors gratefully acknowledge Liela Mendoza, clinical research coordinator in the Blood and Marrow Transplant Clinic at the Tom Baker Cancer Centre, for her assistance in data entry and data cleaning.
[[{"type":"media","view_mode":"media_original","fid":"26626","attributes":{"alt":"","class":"media-image","height":"515","typeof":"foaf:Image","width":"368"}}]]
References
Aizer, A.A., Chen, M.-H., McCarthy, E.P., Mendu, M.L., Koo, S., Wilhite, T.J., . . . Nguyen, P.L. (2013). Marital status and survival in patients with cancer. Journal of Clinical Oncology, 31, 3869–3876. doi:10.1200/JCO.2013.49.6489
Alcorn, S.R., Balboni, M.J., Prigerson, H.G., Reynolds, A., Phelps, A.C., Wright, A.A., . . . Balboni, T.A. (2010). “If God wanted me yesterday, I wouldn’t be here today”: Religious and spiritual themes in patients’ experiences of advanced cancer. Journal of Palliative Medicine, 13, 581–588. doi:10.1089/jpm.2009.0343
Andrykowski, M.A., Bishop, M.M., Hahn, E.A., Cella, D.F., Beaumont, J.L., Brady, M.J., . . . Wingard, J.R. (2005). Long-term health-related quality of life, growth, and spiritual well-being after hematopoietic stem-cell transplantation. Journal of Clinical Oncology, 23, 599–608. doi:10.1200/JCO.2005.03.189
Balboni, M.J., Sullivan, A., Enzinger, A.C., Epstein-Peterson, Z.D., Tseng, Y.D., Mitchell, C.,. . . Balboni, T.A. (2014). Nurse and physician barriers to spiritual care provision at the end of life. Journal of Pain and Symptom Management, 48, 400–410. doi:10.1016/j.jpainsymman.2013.09.020
Balboni, T.A., Vanderwerker, L.C., Block, S.D., Paulk, M.E., Lathan, C.S., Peteet, J.R., & Prigerson, H.G. (2007). Religiousness and spiritual support among advanced cancer patients and associations with end-of-life treatment preferences and quality of life. Journal of Clinical Oncology, 25, 555–560. doi:10.1200/JCO.2006.07.9046
Berger, J.A. (2001). Living the Discipline on a stem cell transplant unit: Spiritual care outcomes among bone marrow transplant survivors. Journal of Health Care Chaplaincy, 11, 83–93. doi:10.1300/j080v11n01_01
Byar, K.L., Eilers, J.E., & Nuss, S.L. (2005). Quality of life 5 or more years post-autologous hematopoietic stem cell transplant. Cancer Nursing, 28, 148–157. doi:10.1097/00002820-200503000-00010
Calman, K.C. (1984). Quality of life in cancer patients—An hypothesis. Journal of Medical Ethics, 10, 124–127. doi:10.1136/jme.10.3.124
Carpenter, J.S., Brockopp, D.Y., & Andrykowski, M.A. (1999). Self-transformation as a factor in the self-esteem and well-being of breast cancer survivors. Journal of Advanced Nursing, 29, 1402–1411. doi:10.1046/j.1365-2648.1999.01027.x
Cella, D.F., & Tulsky, D.S. (1993). Quality of life in cancer: Definition, purpose, and method of measurement. Cancer Investigation, 11, 327–336. doi:10.3109/07357909309024860
Clark, W., & Schellenberg, G. (2006). Who’s religious? Canadian Social Trends, 81, 2–9.
Cohen, M., Headley, J., & Sherwood, G. (2000). Spirituality and bone marrow transplantation: When faith is stronger than fear. International Journal for Human Caring, 4, 40–46.
Costantini, M., & Higginson, I.J. (2007). Experimental and quasi-experimental designs. In J.M. Addington-Hall, E. Bruera, I.J. Higginson, & S. Payne (Eds.), Research Methods in Palliative Care (pp. 87–91). Oxford, UK: Oxford University Press.
Ferrell, B., Grant, M., Schmidt, G.M., Rhiner, M., Whitehead, C., Fonbuena, P., & Forman, S.J. (1992). The meaning of quality of life for bone marrow transplant survivors. Part 1. The impact of bone marrow transplant on quality of life. Cancer Nursing, 15, 153–160. doi:10.1097/00002820-199206000-00001
Fromm, K., Andrykowski, M.A., & Hunt, J. (1996). Positive and negative psychosocial sequelae of bone marrow transplantation: Implications for quality of life assessment. Journal of Behavioral Medicine, 19, 221–240. doi:10.1007/bf01857767
Gaston-Johansson, F., & Foxall, M. (1996). Psychological correlates of quality of life across the autologous bone marrow transplant experience. Cancer Nursing, 19, 170–176. doi:10.1097/00002820-199606000-00003
Graduate Center of the City University of New York. (2001). American religious identification survey, 2001. Retrieved from http://www.gc.cuny.edu/CUNY_GC/media/CUNY-Graduate-Center/PDF/ARIS/ARIS…
King, D.E., & Crisp, J. (2007). Case discussion: Do not neglect the spiritual history. Southern Medical Journal, 100, 426. doi:10.1097/smj.0b013e31803169dd
King, S.D., Fitchett, G., Murphy, P.E., Pargament, K.I., Martin, P.J., Johnson, R.H., . . . Loggers, E.T. (2015). Spiritual or religious struggle in hematopoietic cell transplant survivors. Psycho-Oncology. Advance online publication. doi:10.1002/pon.4029
Kissane, D.W. (2013). Marriage is as protective as chemotherapy in cancer care. Journal of Clinical Oncology, 31, 3852–3853. doi:10.1200/JCO.2013.51.5080
Kristeller, J.L., Zumbrun, C.S., & Schilling, R.F. (1999). ‘I would if I could’: How oncologists and oncology nurses address spiritual distress in cancer patients. Psycho-Oncology, 8, 451–458. doi:10.1002/(sici)1099-1611(199909/10)8:5<451::aid-pon422>3.0.co;2-3
Le, R.Q., Bevans, M., Savani, B.N., Mitchell, S.A., Stringaris K., Koklanaris, E., & Barrett, A.J. (2010). Favorable outcomes in patients surviving 5 or more years after allogeneic hematopoietic stem cell transplantation for hematologic malignancies. Biology of Blood and Marrow Transplantation, 16, 1162–1170. doi:10.1016/j.bbmt.2010.03.005
Lelorain, S., Bonnaud-Antignac, A., & Florin, A. (2010). Long term posttraumatic growth after breast cancer: Prevalence, predictors and relationships with psychological health. Journal of Clinical Psychology in Medical Settings, 17, 14–22. doi:10.1007/s10880-009-9183-6
Maslow, A.H. (1943). A theory of human motivation. Psychological Review, 50, 370–396. doi:10.1037/h0054346
McQuellon, R.P., Russell, G.B., Cella, D.F., Craven, B.L., Brady, M., Bonomi, A., & Hurd, D.D. (1997). Quality of life measurement in bone marrow transplantation: Development of the Functional Assessment of Cancer Therapy–Bone Marrow Transplant (FACT-BMT) scale. Bone Marrow Transplantation, 19, 357–368. doi:10.1038/sj.bmt.1700672
Peterman, A.H., Fitchett, G., Brady, M.J., Hernandez, L., & Cella, D. (2002). Measuring spiritual well-being in people with cancer: The Functional Assessment of Chronic Illness Therapy–Spiritual Well-Being scale (FACIT-Sp). Annals of Behavioral Medicine, 24, 49–58. doi:10.1207/s15324796abm2401_06
Phelps, A.C., Lauderdale, K.E., Alcorn, S., Dillinger, J. Balboni, M.T., Van Wert, M., . . . Balboni, T.A. (2012). Addressing spirituality within the care of patients at the end of life: Perspectives of patients with advanced cancer, oncologists, and oncology nurses. Journal of Clinical Oncology, 30, 2538–2544. doi:10.1200/JCO.2011.40.3766
Pidala, J., Anasetti, C., & Jim, H. (2009). Quality of life after allogeneic hematopoietic cell transplantation. Blood, 114, 7–19. doi:10.1182/blood-2008-10-182592
Reuter, K., Raugust, S., Marschner, N., & Härter, M. (2007). Differences in prevalence rates of psychological distress and mental disorders in inpatients and outpatients with breast and gynaecological cancer. European Journal of Cancer Care, 16, 222–230. doi:10.1111/j.1365-2354.2006.00744.x
Saleh, U.S., & Brockopp, D.Y. (2001). Quality of life one year following bone marrow transplantation: Psychometric evaluation of the quality of life in bone marrow transplant survivors tool. Oncology Nursing Forum, 28, 1457–1464.
Sinclair, S., & Chochinov, H. (2012a). The role of chaplains within oncology interdisciplinary teams. Current Opinion in Supportive and Palliative Care, 6, 259–268. doi:10.1097/SPC.0b013e3283521ec9
Sinclair, S., & Chochinov, H.M. (2012b). Communicating with patients about existential and spiritual issues: SACR-D work. Progress in Palliative Care, 20, 72–78. doi:10.1179/1743291x12y.0000000015
Sinclair, S., & Chochinov, H.M. (2012c). Dignity: A novel path into the spiritual landscape of the human heart. In M. Cobb, C.M. Puchalski, & B. Rumbold (Eds.), Oxford textbook of spirituality in healthcare (pp. 145–149). Oxford, UK: Oxford University Press.
Sinclair, S., McConnell, S., Raffin Bouchal, S., Ager, N., Booker, R., Enns, B., & Fung, T. (2015). Patient and healthcare perspectives on the importance and efficacy of addressing spiritual issues within an interdisciplinary bone marrow transplant clinic: A qualitative study. BMJ Open, 5, e009392. doi:10.1136/bmjopen-2015-009392
Sinclair, S., Mysak, M., & Hagen, N.A. (2009). What are the core elements of oncology spiritual care programs? Palliative and Supportive Care, 7, 415–422. doi:10.1017/S1478951509990423
Sirilla, J., & Overcash, J. (2012). Quality of life (QOL), supportive care, and spirituality in hematopoietic stem cell transplant (HSCT) patients. Supportive Care in Cancer, 21, 1137–1144. doi:10.1007/s00520-012-1637-y
Smith, B.W., Dalen, J., Bernard, J.F., & Baumgartner, K.B. (2008). Posttraumatic growth in non-Hispanic white and Hispanic women with cervical cancer. Journal of Psychosocial Oncology, 26, 91–109. doi:10.1080/07347330802359768
Smith-Stoner, M. (2007). End-of-life preferences for atheists. Journal of Palliative Medicine, 10, 923–928. doi:10.1089/jpm.2006.0197
Tedeschi, R.G., & Calhoun, L.G. (1996). The Posttraumatic Growth Inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress, 9, 455–471. doi:10.1007/bf02103658
Thombre, A., Sherman, A.C., & Simonton, S. (2010). Religious coping and posttraumatic growth among family caregivers of cancer patients in India. Journal of Psychosocial Oncology, 28, 173–188. doi:10.1080/07347330903570537
Ubel, P.A., Loewenstein, G., & Jepson, C. (2003). Whose quality of life? A commentary exploring discrepancies between health state evaluations of patients and the general public. Quality of Life Research, 12, 599–607.
Whedon, M., & Ferrell, B.R. (1994). Quality of life in adult bone marrow transplant patients: Beyond the first year. Seminars in Oncology Nursing, 10, 42–57. doi:10.1016/s0749-2081(05)80044-0
Whitford, H.S., & Olver, I.N. (2012). The multidimensionality of spiritual well-being: Peace, meaning, and faith and their association with quality of life and coping in oncology. Psycho-Oncology, 21, 602–610. doi:10.1002/pon.1937
Widows, M.R., Jacobsen, P.B., Booth-Jones, M., & Fields, K.K. (2005). Predictors of posttraumatic growth following bone marrow transplantation for cancer. Health Psychology, 24, 266–273. doi:10.1037/0278-6133.24.3.266
World Health Organization. (2015). People-centered and integrated health services: An overview of the evidence. Retrieved from http://apps.who.int/iris/bitstream/10665/155004/1/WHO_HIS_SDS_2015.7_en…
Zabora, J., BrintzenhofeSzoc, K., Curbow, B., Hooker, C., & Piantadosi, S. (2001). The prevalence of psychological distress by cancer site. Psycho-Oncology, 10, 19–28. doi:10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.3.co;2-y
Zaza, C., Sellick, S.M., & Hillier, L.M. (2005). Coping with cancer: What do patients do? Journal of Psychosocial Oncology, 23, 55–73. doi:10.1300/j077v23n01_04
About the Author(s)
Sinclair is an assistant professor in the Faculty of Nursing at the University of Calgary; Booker is a nurse practitioner and clinical nurse specialist at the Tom Baker Cancer Centre; Fung is a senior statistical consultant and adjunct assistant professor in the Faculty of Information Technologies, and Raffin-Bouchal is an associate dean and associate professor in the Faculty of Nursing, both at the University of Calgary; Enns is a spiritual care specialist and project manager at the Tom Baker Cancer Centre; Beamer is a research coordinator in the Compassion Research Lab in the Faculty of Nursing at the University of Calgary; and Ager is manager of the Alberta Bone Marrow and Blood Cell Transplant Program at the Tom Baker Cancer Centre, all in Calgary, Alberta, Canada. No financial relationships to disclose. Sinclair, Booker, Fung, Raffin-Bouchal, Enns, and Ager contributed to the conceptualization and design. Sinclair, Fung, Raffin-Bouchal, Enns, and Ager completed the data collection. Sinclair, Booker, and Fung provided statistical support. Sinclair, Booker, Fung, Raffin-Bouchal, and Beamer contributed to the analysis. Booker, Fung, Raffin-Bouchal, Enns, Beamer, and Ager contributed to the manuscript preparation. Sinclair can be reached at sinclair@ucalgary.ca, with copy to editor at ONFEditor@ons.org. Submitted December 2015. Accepted for publication February 19, 2016.

