Evaluation of Online Learning Modules for Improving Physical Activity Counseling Skills, Practices, and Knowledge of Oncology Nurses
Purpose/Objectives: To examine the effectiveness of online learning modules for improving physical activity counseling practices among oncology nurses.
Design: Randomized, controlled trial.
Setting: Online.
Sample: 54 oncology nurses.
Methods: Oncology nurses were randomly assigned to the learning modules group or control group. The learning modules group completed six online learning modules and quizzes focused on physical activity for cancer survivors, general physical activity principles, and motivational interviewing.
Main Research Variables: Percentage of cancer survivors counseled, self-efficacy for physical activity counseling, knowledge of physical activity, and perceived barriers and benefits of physical activity counseling.
Findings: Analyses of covariance revealed no significant difference between the learning modules and control groups in the percentage of cancer survivors that oncology nurses counseled. Significant differences were found in self-efficacy for physical activity counseling and perceived barriers to physical activity counseling at postintervention.
Conclusions: The online learning intervention tested in this study improved some parameters of physical activity counseling but did not increase the percentage of cancer survivors that oncology nurses counseled. Additional pilot work is needed to refine the intervention.
Implications for Nursing: This study suggests the potential utility of an evidence-based online learning strategy for oncology nurses that includes information on physical activity and its benefits in cancer survivorship. The findings offer a framework on how to implement physical activity counseling skills in oncology nursing practice.
Jump to a section
Regular physical activity has been found to be an important supportive care strategy for cancer survivors that has physical and psychosocial benefits during and following treatment. Notably, physical activity has been found in several randomized, controlled trials to improve fatigue, depression, physical function, cardiovascular fitness, muscular strength, and overall quality of life in a wide variety of cancer survivor populations (Buffart, Galvão, Brug, Chinapaw, & Newton, 2014). In addition, growing observational research suggests that regular physical activity is associated with a decrease in cancer mortality among cancer survivors (Li et al., 2016).
Despite the many benefits of physical activity in cancer survivorship, physical activity rates, on average, are low among cancer survivors, with only 22% reporting sufficient physical activity that meets public health physical activity recommendations (Courneya, Katzmarzyk, & Bacon, 2008). Although many factors may contribute to lower rates of physical activity in cancer survivors (e.g., lack of access to appropriate facilities, lack of motivation, safety concerns) (Blaney, Lowe-Strong, Rankin-Watt, Campbell, & Gracey, 2013), greater physical activity participation may occur if more guidance and support were given by healthcare providers (Daley, Bowden, Rea, Billingham, & Carmichael, 2008). In addition, most cancer survivors indicate that they are receptive to receiving physical activity counseling (Forbes, Blanchard, Mummery, & Courneya, 2015) and that such recommendations made by clinicians may increase cancer survivors’ physical activity behavior (Park et al., 2015).
Oncology nurses play an important role in providing survivorship care, including counseling for lifestyle behaviors, such as physical activity (Grant, Economou, & Ferrell, 2010). However, survey evidence suggests that many oncology nurses believe they lack sufficient knowledge to provide effective physical activity counseling to cancer survivors (Anderson, Caswell, Wells, & Steele, 2013; Karvinen, Bruner, & Truant, 2015; Karvinen, McGourty, Parent, & Walker, 2012). For example, a survey of oncology nurses by Karvinen et al. (2012) notes that being unsure about what to recommend and having concerns about the safety of physical activity for cancer survivors are the most important negative correlates of physical activity counseling. In addition, oncology professionals have indicated they could benefit from lifestyle behavior counseling and are interested in receiving training in physical activity and other lifestyle behaviors (Anderson et al., 2013; Karvinen et al., 2015; Sarna et al., 2000).
In general, online learning strategies for healthcare professionals have been found to be an effective means of delivering continuing professional development and lifelong learning, yet allow flexibility to participate during times that are convenient for the learner (Koch, 2014; Riley & Schmidt, 2016; Southernwood, 2008). In nursing settings, several reviews suggest that online learning is as effective as traditional classroom-based instruction for acquiring clinical skills and has a similar level of learner satisfaction (Bloomfield, While, & Roberts, 2008; Cook et al., 2010; Koch, 2014). Teaching methods that employ strategies including the provision of feedback and the use of case studies have been found to result in several positive learner outcomes, such as improvement in clinical practice, confidence, motivation, and problem solving (Clynes & Raftery, 2008; Dowd & Davidhizar, 1999; Popil, 2011). For example, a number of online learning interventions have been found to be effective in enhancing nurses’ counseling skills for a variety of clinical areas, including reducing secondhand smoke exposure for children (Jones & McEwen, 2015), providing spiritual care (Petersen et al., 2017), and improving patient satisfaction with pain management (Schroeder et al., 2016).
The purpose of this study was to examine the effectiveness of an online learning intervention for improving oncology nurses’ physical activity counseling practices. Oncology nurses receiving the intervention were hypothesized to demonstrate an increase in the percentage of survivors they counseled about physical activity. The secondary purposes were to explore changes in oncology nurses’ self-efficacy for physical activity counseling, knowledge about physical activity, perceived barriers to physical activity counseling, and perceived benefits of physical activity counseling for cancer survivors. The authors expected that oncology nurses receiving the intervention would indicate increases in these factors related to physical activity counseling.
Methods
Design
Study approval was granted by the research ethics board at Nipissing University in North Bay, Ontario, Canada. The study was a two-armed, prospective, randomized, controlled trial. Study participants were randomly assigned to either the learning modules group or a control group using a computer-generated program in a 1:1 ratio in blocks of four. To create the allocation sequence, a research assistant not associated with the study assembled the results into a series of sequentially numbered opaque envelopes. Each consecutive envelope was opened by a member of the research team after each new participant completed baseline measures. Results of the randomization were revealed to participants via email.
Sample
Participants were recruited through emails to about 800 members of the Canadian Association of Nurses in Oncology (CANO) and to a random selection of 2,000 members of the Oncology Nursing Society (ONS). CANO and InFocus Marketing (on behalf of ONS) performed the email blasts. The emails provided a description of the study and invited interested participants to contact the researchers. Eligibility criteria included (a) being English speaking; (b) being employed as a medical, radiation, surgical, or bone marrow transplantation oncology nurse, advanced practice nurse, or nurse navigator; (c) currently providing care to cancer survivors in a clinical setting; and (d) residing in Canada or the United States. Participants provided written consent before commencing the study. All baseline and postintervention assessments were conducted via online survey.
Participants were recruited for the study from November 2012 to July 2013. A total of 106 inquiry emails were received from interested oncology nurses. Of these, 59 oncology nurses were recruited to the study, and 54 completed all baseline measures and were randomized (27 each to the learning modules and control groups). One participant (control group) failed to complete post-test measures; however, baseline data for that participant were still included in the analyses. All participants in the learning modules group completed the quizzes that were at the end of each module. Figure 1 displays the flow of the participants through the study. 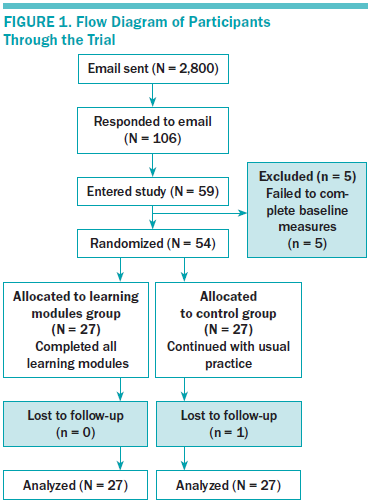
Learning Modules Group
Participants randomized to the learning modules group completed a set of online learning modules designed to improve physical activity knowledge and counseling skills to support cancer survivors. The learning modules were based on the social cognitive theory (SCT) constructs of self-efficacy (confidence in providing physical activity counseling), behavioral capacity (knowledge and skills related to physical activity counseling), outcome expectations (anticipated outcomes of physical activity counseling), and situation and environment (perceived barriers to physical activity counseling). SCT is a versatile model of human behavior that highlights the capacity for self-regulation (Bandura, 1986). It has been used as the framework for a wide variety of interventions that require changing behavior, including training individuals to perform counseling behaviors (Larson, 1998). Each of the learning modules was developed to target one or more of the SCT constructs in an effort to improve physical activity counseling.
The learning modules consisted of six individual modules, each completed during a two-week period for a 12-week duration. Each module took about 30 minutes to complete. The content of the modules included case studies, sample dialogues, and video links to examples (e.g., samples of motivational interviewing dialogue). At the end of each module, participants completed a 10-item online quiz based on the content of the module. Feedback was provided regarding correct and incorrect answers on the quiz. Participants had to complete each quiz before being allowed access to the next module. The themes of the modules were (a) benefits of physical activity in cancer survivorship, (b) physical activity guidelines for cancer survivors, (c) motivational interviewing, (d) motivational strategies for behavior change, (e) strategies for keeping active, and (f) barriers to physical activity counseling. The modules and quizzes were all developed by the authors and evaluated for content by a panel of 10 external evaluators, including oncology nurses, physical activity experts, and physical activity and cancer researchers.
Control Group
Participants assigned to the control group were provided with a list of reputable, publicly available websites concerning physical activity and cancer (i.e., American Cancer Society and American College of Sports Medicine). After all measures were collected, control group participants were given access to the learning modules.
Measures
Demographic and professional variables (e.g., age, number of years practicing oncology nursing, geographic region, ethnicity) were assessed by self-report at baseline.
Physical activity counseling practice was assessed by one item based on scales developed by Sherman and Hershman (1993) and Walsh, Swangard, Davis, and McPhee (1999) to assess exercise counseling practices of physicians. The stem of the item was, “What percentage of cancer survivors that you encounter do you provide physical activity counseling to (when appropriate)?” The possible range of the scale was 0%–100%.
Self-efficacy for physical activity counseling was measured using a modified version of the Helping Skill Self-Efficacy scale from the Counselor Activity Self-Efficacy Scales (CASES) (Lent, Hill, & Hoffman, 2003). For the current study, the Helping Skill Self-Efficacy scale was modified to be applicable to self-efficacy for physical activity counseling instead of general counseling, specifically by removal of the “immediacy,” “self-disclosure,” “self-disclosure for exploration,” and “intentional silence” items. In addition, examples were changed to reflect physical activity counseling. The modified CASES scale consisted of 11 items, each rated on a 10-point Likert-type scale ranging from 1 (no confidence) to 10 (complete confidence). The mean of the 11 items was calculated and used as the final score. The CASES scales have been found to be internally reliable and stable during a two-week test-retest period, as well as to have good convergent and discriminant validity (Lent et al., 2003). In the current study, internal consistency was found to have a Cronbach alpha of 0.96.
Perceived barriers to physical activity counseling were assessed by asking participants to rate several potential barriers to physical activity counseling (lack of time, unsure what to recommend, unsure that physical activity is safe, unsure that physical activity can help, cancer survivors are not interested) on a five-item, five-point Likert-type scale ranging from 1 (not at all) to 5 (very much). These items were based on two studies assessing barriers to physical activity promotion by oncologists (Karvinen, DuBose, Carney, & Allison, 2010) and oncology nurses (Karvinen et al., 2012). The mean of the items was used as the measure. Internal consistency for the scale was found to have a Cronbach alpha of 0.66.
Perceived benefits of physical activity counseling for cancer survivors were determined by asking participants to rate four items on a six-point Likert-type scale ranging from 1 (not at all) to 6 (very much) on how beneficial they felt physical activity counseling was for cancer survivors. These items were derived from previous studies of oncology healthcare providers’ perceived benefits of physical activity for cancer survivors (Karvinen et al., 2010, 2012). The mean of the four items was used as the final score for this measure. Internal reliability for the scale in the current study was found to have a Cronbach alpha of 0.71.
Knowledge about physical activity for cancer survivors was assessed by a 13-item survey modeled after the knowledge subscale (section 2) of the Exercise Teaching Questionnaire (Ruby, Blainey, Haas, & Patrick, 1993). The Exercise Teaching Questionnaire was designed to assess diabetes educators’ practices in teaching exercise to adults with type 2 diabetes. This subscale specifically evaluates knowledge about physical activity guidelines, safety, and effects, with four fixed alternative responses per item. The survey in the current study was modified to assess general knowledge concerning physical activity and specific knowledge of physical activity and cancer. Knowledge about physical activity for cancer survivors was determined by totaling the number of correctly answered items (range = 0–13).
Knowledge retention from modules was determined by quizzes that were included at the end of each of the six modules. Each quiz consisted of 10 multiple-choice items, each with four fixed alternative responses, that tested the content of the module. Quiz scores for each module were determined by totaling the number of correct answers (range = 0–10).
Participants’ physical activity behavior was measured by a modified version of the leisure score index (LSI) of the Godin Leisure-Time Exercise Questionnaire (Godin, Jobin, & Bouillon, 1986). In the current study, the modified LSI measured the average frequency of moderate intensity, vigorous intensity, and resistance training weekly exercise minutes in a typical week in the past month. The LSI has been found to indicate acceptable concurrent validity when compared with accelerometer and VO2 max, and acceptable one-month test-retest reliability (Jacobs, Ainsworth, Hartman, & Leon, 1993). Separate scores for average weekly minutes of moderate intensity activity, vigorous intensity activity, combined moderate to vigorous intensity activity, and resistance training were calculated.
Sample Size Calculation and Statistical Analyses
To detect a large effect with a power of 0.8 at a two-tailed alpha at less than 0.05, 26 participants were needed in each condition (Cohen, 1992). All analyses were conducted using SPSS®, version 23.0. Demographic, professional, and physical activity data were analyzed using descriptive statistics. Comparisons among baseline demographic, professional, and physical activity characteristics were examined by independent samples t tests for continuous data and by chi-square analyses for categorical data. Means and standard deviations of the outcome variables were determined using descriptive statistics. Analyses of covariance (ANCOVAs) were used to compare postintervention primary and secondary outcome variables between the learning modules and control groups, controlling for baseline values for each corresponding measure.
Results
No significant differences were observed among demographic, professional, and physical activity variables between the learning modules and control groups at baseline (see Table 1). The mean age was 45.4 years (SD = 10.8) and the mean number of years practicing was 19.5 (SD = 11.4). The mean number of weekly moderate to vigorous intensity physical activity minutes accumulated by oncology nurses at baseline was 142.1 (SD = 132.6). Mean quiz scores on the modules are displayed in Table 2. Average scores ranged from 7.76 (SD = 1.96) (module 3) to 9.21 (SD = 1.06) (module 6).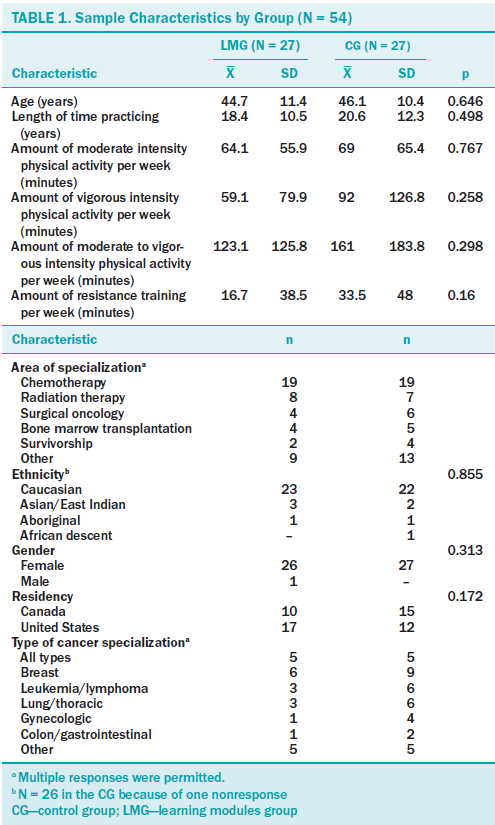
Means and standard deviations of the outcome variables at baseline and postintervention for the learning modules and control groups are displayed in Table 3. An ANCOVA, controlling for baseline score, indicated no significant effect of group on physical activity counseling practice (F[1, 52] = 0.706, p = 0.405, 95% confidence interval [CI] [–7.81, –19.06]). Two separate ANCOVAs, controlling for baseline scores, revealed a significant effect of group in favor of the learning modules group on (a) self-efficacy for physical activity counseling at postintervention (F[1,52] = 7.87, p < 0.001, 95% CI [0.26, –1.6]) and (b) perceived barriers to physical activity counseling at postintervention (F[1,52] = 6.6, p < 0.01, 95% CI [–1.1, –0.13]). All other outcomes favored the learning modules group but were not statistically significant (p > 0.05) (see Table 4). 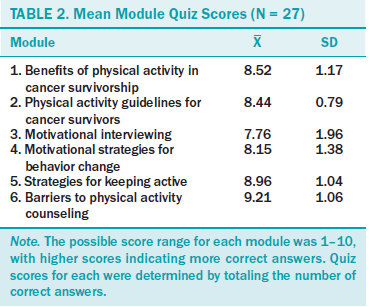
Discussion
The purpose of this study was to examine the effectiveness of an online learning intervention for improving physical activity counseling skills and practices in oncology nurses. Results indicated improvements in self-efficacy and reduced barriers for providing physical activity counseling in oncology nurses in the learning modules group compared to the control group during the intervention. No significant changes were observed in physical activity counseling practice, knowledge about physical activity for cancer survivors, or perceived benefits of physical activity counseling between the learning modules group and the control group at postintervention; however, all changes favored the learning modules group. 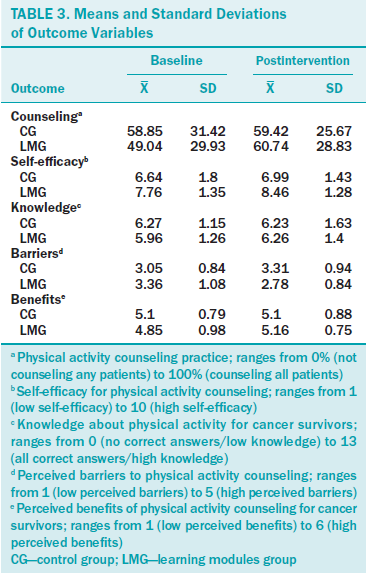
Contrary to the authors’ hypotheses, the learning modules intervention did not result in a significant change in the percentage of cancer survivors who oncology nurses counseled about physical activity. However, nonsignificant improvements were observed in the learning modules group, with no change in the control group. This finding contrasts with previous research that has demonstrated the effectiveness of online learning interventions in changing nurses’ behaviors related to pain assessment (Habich & Letizia, 2015; Phillips, Heneka, Hickman, Lam, & Shaw, 2014), infection prevention (Labeau, 2013), and rapid HIV testing (Knapp, Chan, Anaya, & Goetz, 2011). Physical activity counseling may require more complex interactions than more standard types of practice behaviors tested in previous interventions and, consequently, necessitates a more extensive type of learning intervention to be effective. Alternatively, oncology nurses in this study may have experienced substantial barriers, such as lack of time (Karvinen et al., 2012; Turin, 2015), that prevented them from counseling a greater number of survivors on physical activity, despite exposure to the intervention. Because most nurses reported practicing within a treatment setting where the emphasis is on supporting survivors to manage their treatment, often at the expense of health promotion activities, opportunities to provide physical activity counseling may have been limited by the biomedical disease-focused model of care. The social, political, and economic structures and contexts within which nurses care for patients have been shown to constrain their agency to enact aspects of care, even when they possess the knowledge, skills, and self-efficacy to deliver these aspects of care (Varcoe & Rodney, 2009). 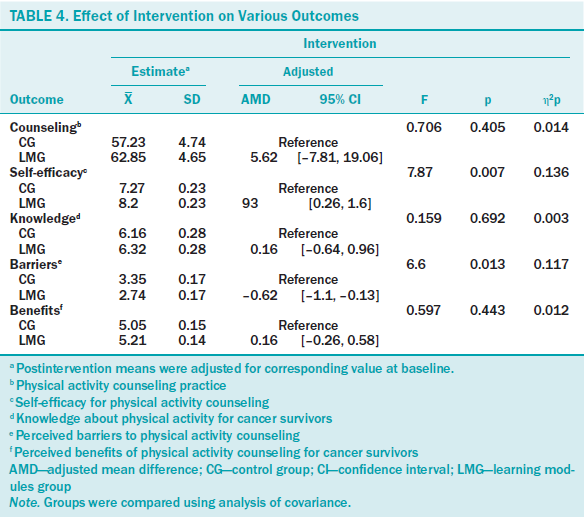
The significant increase in self-efficacy for providing physical activity counseling in the learning modules group compared to the control group during the intervention was as hypothesized and consistent with previous research of interventions designed to change clinicians’ practice behaviors (Edwards, Stapleton, Williams, & Ball, 2015; Jones & McEwen, 2015; Malan, Mash, & Everett-Murphy, 2015). For example, Edwards et al. (2015) found that, after attending a one-day motivational interviewing workshop, nurses’ confidence in their ability to provide counseling for healthy eating and physical activity increased compared to a control group. In addition, basic behavioral research suggests that provision of information to individuals in laboratory settings increases their confidence in making judgments (Tsai, Klayman, & Hastie, 2008). The significant increase in self-efficacy observed in the current study is meaningful, given the important role self-efficacy has as a precondition for behavior change and its influence on the amount of effort expended and perseverance for pursuing behavior, even in the face of adverse obstacles (Bandura, 1977). Increased self-efficacy for providing physical activity counseling is important because of its potential effect on oncology nurses’ intention for providing physical activity counseling.
Also, as expected, and consistent with previous research (Jonsdottir et al., 2016; Malan et al., 2015), a decrease in perceived barriers to providing physical activity counseling was noted in the learning modules group. This finding was in accordance with previous research that has suggested that educational interventions can reduce practitioners’ perceived barriers in providing sexual health care (Jonsdottir et al., 2016) and increase confidence in overcoming barriers to providing health behavior change counseling (Malan et al., 2015). The intervention may have reduced perceived barriers because it improved nurses’ physical activity counseling skills—a factor that has been found in previous research to be a prominent barrier to providing physical activity counseling to cancer survivors (Karvinen et al., 2010, 2012).
Unexpectedly, knowledge about physical activity did not significantly change in the learning modules group during the intervention compared to the control group. Previous research has indicated significant increases in knowledge in spiritual care (Petersen et al., 2017) and pain assessment (Schroeder et al., 2016) among nurses after exposure to online learning interventions. In the current study, quiz scores at the end of each module were moderately high, suggesting that learning had occurred at least immediately after completing the module. The items that measured knowledge may not have been sensitive enough to capture changes in physical activity and cancer knowledge, or perhaps long-term retention of material was not accomplished.
Previous research has found positive changes in clinicians’ attitudes toward providing counseling to patients concerning smoking cessation (Kerr, Whyte, Watson, Tolson, & McFadyen, 2011) and breast screening (Bryan, Estrada, Castigilioni, & Snyder, 2015) after participation in training interventions. In contrast, exposure to the learning modules in the current study did not result in changes in perceived benefits of physical activity counseling. However, this is not surprising because a ceiling effect may have occurred; the mean scores on the perceived benefits of physical activity counseling measure were very high at baseline (4.85 and 5.1 for the learning modules and control groups, respectively, on a six-point scale). Participants who valued physical activity counseling were most likely to be recruited into the study, reflecting the high scores at baseline and postintervention.
Collectively, the results were not fully supportive of the theory that informed the study (SCT). Although the intervention resulted in increased self-efficacy and decreased perceived barriers, these changes did not lead to an increase in physical activity counseling. However, participation in the modules may have improved the quality of the physical activity counseling provided as a result of improved self-efficacy and fewer perceived barriers. In previous research, self-efficacy has been found to be an important moderator of adopting more effective clinical practice, including lifestyle behavior counseling (Sargeant, Valli, Ferrier, & MacLeod, 2008). Alternatively, the time interval of the study may have been insufficient to observe changes in the volume of physical activity counseling provided to cancer survivors. A larger study that examines the quality of physical activity counseling and changes during a longer time period could provide additional understanding of the effect of the intervention on physical activity counseling.
Findings from this study support the potential effectiveness of online learning strategies for improving oncology nurses’ physical activity counseling skills. Previous studies have indicated that oncology nurses may lack the knowledge and skills to provide physical activity counseling to cancer survivors and are eager to receive further training (Karvinen et al., 2012, 2015). Although published literature on physical activity in cancer survivorship is available for clinicians to access, busy oncology nurses may have difficulty sifting through the increasingly large volume of cancer care literature for articles that are relevant to their practice (Bertulis, 2008). In addition, most healthcare professionals receive very little formal education in physical activity (Kris-Etherton et al., 2014). As a result, online learning opportunities that are based on evidence, are concise, and can be accessed regardless of geographic location and within a flexible time frame may be beneficial for improving oncology nurses’ physical activity counseling practice.
Limitations
Several limitations with the current study are worth noting. The participants were likely a highly motivated sample of oncology nurses who valued physical activity and may not have been representative of oncology nurses as a whole. Despite a potential bias in the sample, the demographic and professional characteristics (age, number of years practicing nursing, gender, ethnicity) of the sample are similar to those of oncology nurses in previous surveys conducted in Canada and the United States (Helft, Chamness, Terry, & Uhrich, 2011; Karvinen et al., 2012, 2015). In addition, although the mean physical activity level was fairly high, the variability was also high, suggesting that a wide range of physical activity levels was represented in the sample. An additional limitation is that several of the scales used in the study were developed by the researchers, and although tested for face validity and internal consistency, the scales were not tested for further validity and reliability. The measure of physical activity counseling was a self-report, single-item measure, which may be subject to social desirability bias and has limitations regarding psychometric evaluation. Also, the sample size was small, which may have limited power to detect smaller differences between the groups. However, because the authors adjusted for baseline value, they were able to increase power by substantially more than what was estimated from the sample size calculation (Cohen, 1992).
Implications for Nursing
This study has implications for nursing practice. The findings suggest the utility of evidence-based online learning strategies that provide information on the benefits of physical activity on cancer survivorship and offer strategies on how to implement health behavior change counseling skills in improving physical activity counseling skills in oncology nurses. The findings from the current study, and from previous research, further highlight the need to address barriers that possibly impede physical activity counseling that cannot be addressed by educational strategies, such as lack of time (Karvinen et al., 2012; Turin, 2015). Future studies should examine the impact of social, political, economic, and other relevant healthcare system structures and contexts on nurses’ ability to deliver physical activity counseling to cancer survivors to optimize opportunities for survivors to receive this important health promotion support. 
Conclusion
The online learning intervention evaluated in this study may have use for improving oncology nurses’ self-efficacy for providing physical activity counseling and reducing their perceived barriers to physical activity counseling. However, the percentage of cancer survivors that oncology nurses counseled about physical activity did not change during the intervention, suggesting that further refinement and testing of the intervention strategy may be warranted. Ultimately, future research could test longitudinally the impact of the intervention on cancer survivors’ physical activity levels, quality of life, and survival.
[[{"type":"media","view_mode":"media_original","fid":"36641","attributes":{"alt":"","class":"media-image","height":"520","typeof":"foaf:Image","width":"367"}}]]
About the Author(s)
Karvinen is an associate professor in the School of Physical and Health Education at Nipissing University in North Bay, Ontario; Balneaves is an associate professor in the College of Nursing and Faculty of Health Sciences at the University of Manitoba in Winnipeg; Courneya is a professor in the Faculty of Physical Education and Recreation at the University of Alberta in Edmonton; Perry is a professor in the Faculty of Health Disciplines at Athabasca University in Alberta; Truant is a doctoral candidate in the School of Nursing at the University of British Columbia in Vancouver; and Vallance is a professor in the Faculty of Health Disciplines at Athabasca University, all in Canada. During the writing of this article, Truant was supported by the School of Nursing at the University of British Columbia. Karvinen, Balneaves, Courneya, and Truant provided the analysis. Karvinen and Balneaves completed the data collection. Karvinen and Vallance provided statistical support. All authors contributed to the conceptualization and design and the manuscript preparation. Karvinen can be reached at kristinak@nipissingu.ca, with copy to editor at ONFEditor@ons.org. Submitted December 2016. Accepted for publication May 1, 2017.
References
Anderson, A.S., Caswell, S., Wells, M., & Steele, R.J. (2013). Obesity and lifestyle advice in colorectal cancer survivors—How well are clinicians prepared? Colorectal Disease, 15, 949–957. https://doi.org/10.1111/codi.12203
Bandura, A. (1977). Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84, 191–215.
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice Hall.
Bertulis, R. (2008). Barriers to accessing evidence-based information. Nursing Standard, 22, 35–39. https://doi.org/10.7748/ns2008.05.22.36.35.c6541
Blaney, J.M., Lowe-Strong, A., Rankin-Watt, J., Campbell, A., & Gracey, J.H. (2013). Cancer survivors’ exercise barriers, facilitators and preferences in the context of fatigue, quality of life and physical activity participation: A questionnaire-survey. Psycho-Oncology, 22, 186–194. https://doi.org/10.1002/pon.2072
Bloomfield, J.G., While, A.E., & Roberts, J.D. (2008). Using computer assisted learning for clinical skills education in nursing: Integrative review. Journal of Advanced Nursing, 63, 222–235. https://doi.org/10.1111/j.1365-2648.2008.04653.x
Bryan, T.J., Estrada, C.A., Castiglioni, A., & Snyder, E.D. (2015). Impact of an educational intervention on provider knowledge, attitudes, and comfort level regarding counseling women ages 40–49 about breast cancer screening. Journal of Multidisciplinary Healthcare, 8, 209–216. https://doi.org/10.2147/JMDH.S80337
Buffart, L.M., Galvão, D.A., Brug, J., Chinapaw, M.J., & Newton, R.U. (2014). Evidence-based physical activity guidelines for cancer survivors: Current guidelines, knowledge gaps and future research directions. Cancer Treatment Reviews, 40, 327–340. https://doi.org/10.1016/j.ctrv.2013.06.007
Clynes, M.P., & Raftery, S.E. (2008). Feedback: An essential element of student learning in clinical practice. Nurse Education in Practice, 8, 405–411. https://doi.org/10.1016/j.nepr.2008.02.003
Cohen, J. (1992). A power primer. Psychological Bulletin, 112, 155–159.
Cook, D.A., Levinson, A.J., Garside, S., Dupras, D.M., Erwin, P.J., & Montori, V.M. (2010). Instructional design variations in internet-based learning for health professions education: A systematic review and meta-analysis. Academic Medicine, 85, 909–922. https://doi.org/10.1097/ACM.0b013e3181d6c319
Courneya, K.S., Katzmarzyk, P.T., & Bacon, E. (2008). Physical activity and obesity in Canadian cancer survivors: Population-based estimates from the 2005 Canadian Community Health Survey. Cancer, 112, 2475–2482. https://doi.org/10.1002/cncr.23455
Daley, A.J., Bowden, S.J., Rea, D.W., Billingham, L., & Carmichael, A.R. (2008). What advice are oncologists and surgeons in the United Kingdom giving to breast cancer patients about physical activity? International Journal of Behavioral Nutrition and Physical Activity, 5, 46. https://doi.org/10.1186/1479-5868-5-46
Dowd, S.B., & Davidhizar, R. (1999). Using case studies to teach clinical problem-solving. Nurse Educator, 24, 42–46.
Edwards, E.J., Stapleton, P., Williams, K., & Ball, L. (2015). Building skills, knowledge and confidence in eating and exercise behavior change: Brief motivational interviewing training for healthcare providers. Patient Education and Counseling, 98, 674–676. https://doi.org/10.1016/j.pec.2015.02.006
Forbes, C.C., Blanchard, C.M., Mummery, W.K., & Courneya, K.S. (2015). A comparison of physical activity preferences among breast, prostate, and colorectal cancer survivors in Nova Scotia, Canada. Journal of Physical Activity and Health, 12, 823–833. https://doi.org/10.1123/jpah.2014-0119
Godin, G., Jobin, J., & Bouillon, J. (1986). Assessment of leisure time exercise behavior by self-report: A concurrent validity study. Canadian Journal of Public Health, 77, 359–362.
Grant, M., Economou, D., & Ferrell, B.R. (2010). Oncology nurse participation in survivorship care. Clinical Journal of Oncology Nursing, 14, 709–715. https://doi.org/10.1188/10.CJON.709-715
Habich, M., & Letizia, M. (2015). Pediatric pain assessment in the emergency department: A nursing evidence-based practice protocol. Pediatric Nursing, 41, 198–202.
Helft, P.R., Chamness, A., Terry, C., & Uhrich, M. (2011). Oncology nurses’ attitudes toward prognosis-related communication: A pilot mailed survey of Oncology Nursing Society members. Oncology Nursing Forum, 38, 468–474. https://doi.org/10.1188/11.ONF.468-474
Jacobs, D.R., Jr., Ainsworth, B.E., Hartman, T.J., & Leon, A.S. (1993). A simultaneous evaluation of 10 commonly used physical activity questionnaires. Medicine and Science in Sports and Exercise, 25, 81–91.
Jones, L.L., & McEwen, A. (2015). Evaluating an online training module on protecting children from secondhand smoke exposure: Impact on knowledge, confidence and self-reported practice of health and social care professionals. BMC Public Health, 15, 1132. https://doi.org/10.1186/s12889-015-2488-5
Jonsdottir, J.I., Zoëga, S., Saevarsdottir, T., Sverrisdottir, A., Thorsdottir, T., Einarsson, G.V., . . . Fridriksdottir, N. (2016). Changes in attitudes, practices and barriers among oncology health care professionals regarding sexual health care: Outcomes from a 2-year educational intervention at a university hospital. European Journal of Oncology Nursing, 21, 24–30. https://doi.org/10.1016/j.ejon.2015.12.004
Karvinen, K.H., Bruner, B., & Truant, T. (2015). Lifestyle counseling practices of oncology nurses in the United States and Canada. Clinical Journal of Oncology Nursing, 19, 690–696. https://doi.org/10.1188/15.CJON.690-696
Karvinen, K.H., DuBose, K.D., Carney, B., & Allison, R.R. (2010). Promotion of physical activity among oncologists in the United States. Journal of Supportive Oncology, 8, 35–41.
Karvinen, K.H., McGourty, S., Parent, T., & Walker, P.R. (2012). Physical activity promotion among oncology nurses. Cancer Nursing, 35, E41–E48. https://doi.org/10.1097/NCC.0b013e31822d9081
Kerr, S., Whyte, R., Watson, H., Tolson, D., & McFadyen, A.K. (2011). A mixed-methods evaluation of the effectiveness of tailored smoking cessation training for healthcare practitioners who work with older people. Worldviews on Evidence-Based Nursing, 8, 177–186. https://doi.org/10.1111/j.1741-6787.2011.00219.x
Knapp, H., Chan, K., Anaya, H.D., & Goetz, M.B. (2011). Interactive internet-based clinical education: An efficient and cost-savings approach to point-of-care test training. Telemedicine and e-Health, 17, 335–340. https://doi.org/10.1089/tmj.2010.0187
Koch, L.F. (2014). The nursing educator’s role in e-learning: A literature review. Nurse Education Today, 34, 1382–1387. https://doi.org/10.1016/j.nedt.2014.04.002
Kris-Etherton, P.M., Akabas, S.R., Bales, C.W., Bistrian, B., Braun, L., Edwards, M.S., . . . Van Horn, L. (2014). The need to advance nutrition education in the training of health care professionals and recommended research to evaluate implementation effectiveness. American Journal of Clinical Nutrition, 99(Suppl. 5), 1153S–1166S. https://doi.org/10.3945/ajcn.113.073502
Labeau, S.O. (2013). Is there a place for e-learning in infection prevention? Australian Critical Care, 26, 167–172. https://doi.org/10.1016/j.aucc.2013.10.002
Larson, L.M. (1998). The social cognitive model of counselor training. Counseling Psychologist, 26, 219–273. https://doi.org/10.1177/0011000098262002
Lent, R.W., Hill, C.E., & Hoffman, M.A. (2003). Development and validation of the counselor activity self-efficacy scales. Journal of Counseling Psychology, 50, 97–108.
Li, T., Wei, S., Shi, Y., Pang, S., Qin, Q, Yin, J., . . . Liu, L. (2016). The dose-response effect of physical activity on cancer mortality: Findings from 71 prospective cohort studies. British Journal of Sports Medicine, 50, 339–345. https://doi.org/10.1136/bjsports-2015-094927
Malan, Z., Mash, R., & Everett-Murphy, K. (2015). Qualitative evaluation of primary care providers’ experiences of a training programme to offer brief behaviour change counseling on risk factors for non-communicable diseases in South Africa. BMC Family Practice, 16, 101. https://doi.org/10.1186/s12875-015-0318-6
Park, J.-H., Lee, J., Oh, M., Park, H., Chae, J., Kim, D.-I., . . . Jeon, J.Y. (2015). The effect of oncologists’ exercise recommendations on the level of exercise and quality of life in survivors of breast and colorectal cancer: A randomized controlled trial. Cancer, 121, 2740–2748. https://doi.org/10.1002/cncr.29400
Petersen, C.L., Callahan, M.F., McCarthy, D.O., Hughes, R.G., White-Traut, R., & Bansal, N.K. (2017). An online educational program improves pediatric oncology nurses’ knowledge, attitudes, and spiritual care competence. Journal of Pediatric Oncology Nursing, 34, 130–139. https://doi.org/10.1177/1043454216646542
Phillips, J.L., Heneka, N., Hickman, L., Lam, L., & Shaw, T. (2014). Impact of a novel online learning module on specialist palliative care nurses’ pain assessment competencies and patients’ reports of pain: Results from a quasi-experimental pilot study. Palliative Medicine, 28, 521–529. https://doi.org/10.1177/0269216314527780
Popil, I. (2011). Promotion of critical thinking by using case studies as teaching method. Nurse Education Today, 31, 204–207. https://doi.org/10.1016/j.nedt.2010.06.002
Riley, K., & Schmidt, D. (2016). Does online learning click with rural nurses? A qualitative study. Australian Journal of Rural Health, 24, 265–270. https://doi.org/10.1111/ajr.12263
Ruby, K.L., Blainey, C.A., Haas, L.B., & Patrick, M. (1993). The knowledge and practices of registered nurse, certified diabetes educators: Teaching elderly clients about exercise. Diabetes Educator, 19, 299–306.
Sargeant, J., Valli, M., Ferrier, S., & MacLeod, H. (2008). Lifestyle counseling in primary care: Opportunities and challenges for changing practice. Medical Teacher, 30, 185–191. https://doi.org/10.1080/01421590701802281
Sarna, L.P., Brown, J.K., Lillington, L., Rose, M., Wewers, M.E., & Brecht, M.L. (2000). Tobacco interventions by oncology nurses in clinical practice: Report from a national survey. Cancer, 89, 881–889.
Schroeder, D.L., Hoffman, L.A., Fioravanti, M., Medley, D.P., Zullo, T.G., & Tuite, P.K. (2016). Enhancing nurses’ pain assessment to improve patient satisfaction. Orthopedic Nursing, 35, 108–117. https://doi.org/10.1097/NOR.0000000000000226
Sherman, S.E., & Hershman, W.Y. (1993). Exercise counseling: How do general internists do? Journal of General Internal Medicine, 8, 243–248.
Southernwood, J. (2008). Distance learning: The future of continuing professional development. Community Practitioner, 81, 21–23.
Tsai, C.I., Klayman, J., & Hastie, R. (2008). Effects of amount of information on judgment accuracy and confidence. Organizational Behavior and Human Decision Processes, 107, 97–105.
Turin, R. (2015). Physical activity prescriptions in healthy populations: Resources for Canadian nurse practitioners. Nurse Practitioner, 40, 45–54. https://doi.org/10.1097/01.NPR.0000459731.77403.c1
Varcoe, C., & Rodney, P. (2009). Constrained agency: The social structure of nurses’ work. In B.S. Bolaria & H. Dickinson (Eds.), Health, illness, and health care in Canada (4th ed., pp. 122–151). Scarborough, ON: Nelson Thomson Learning.
Walsh, J.M., Swangard, D.M., Davis, T., & McPhee, S.J. (1999). Exercise counseling by primary care physicians in the era of managed care. American Journal of Preventive Medicine, 16, 307–313.

